Pituitary abscess (PA) is a rare but potentially life-threatening condition characterized by an accumulation of pus within the pituitary gland. The diagnosis of PA is often challenging due to its nonspecific clinical presentation and radiological findings that overlap with other sellar masses, such as pituitary adenomas or cysts [1]. This diagnostic difficulty can lead to delayed or inappropriate treatment, increasing the risk of severe complications including visual impairment, hypopituitarism, and, in some cases, death.
Advances in imaging techniques and surgical interventions have improved the outcomes for PA patients. However, the condition remains difficult to diagnose preoperatively, and there is no consensus on the optimal treatment regimen [2]. Surgical drainage followed by antibiotic therapy is the most commonly recommended approach, yet the choice of surgical technique and the duration of antibiotic therapy are subjects of ongoing debate.
The significance of our case report lies in highlighting the diagnostic challenges and effective treatment strategies for PA. By analyzing 2 cases of primary PA successfully treated with endoscopic transsphenoidal surgery, we aim to provide insights into the clinical management of this rare condition and emphasize the importance of considering PA in the differential diagnosis of sellar masses.
A 61-year-old man was admitted to the neurosurgery department with symptoms of dizziness, fatigue, seizures for 6 months, and blurred vision for 3 days. He had a history of craniotomy for brain injury 20 years ago and was a chronic smoker (20 cigarettes daily for 40 years). Brain magnetic resonance (MRI) revealed a sellar isointense mass with uniform enhancement and a softening spot-encephalomalacia on the left temporal lobe along with right maxillary and ethmoid sinusitis.
The patient had no fever. His temperature was 36.6°C, and his blood pressure was 132/76 mmHg. There were no acromegalic, Cushingoid, or eunuchoid features. Visual assessment showed no abnormalities. His cardiovascular system was essentially normal. Chest radiography showed no sarcoidosis or tuberculosis. His abdomen was soft and free of lumps.
Laboratory findings: Moderate anemia (hemoglobin: 80 g/l, hematocrit: 25.20%), hypothyroidism (free T4: 1.08 pmol/l, free T3: 2.63 pmol/l, TSH: 2.76 mIU/l), low serum GH (0.121 ng/ml), normal serum prolactin (8.99 ng/ml), low free testosterone (6.99 pmol/l), high FSH (10.18 mIU/ml), and high LH (10.13 mIU/ml). Serum sodium and potassium were normal. The detailed information about the laboratory findings is shown in Table I.
Table I
Laboratory findings for case 1
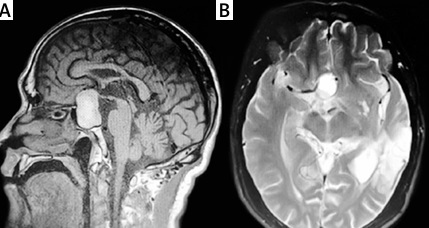
Imaging: MRI revealed a sellar and suprasellar mass measuring 4.0 × 1.5 × 2.0 cm. T1- and T2-weighted images showed hyperintense and hypointense signals respectively. Gadolinium enhancement showed uniform enhancement. The normal pituitary gland had disappeared, and only the posterior bright spot and pituitary stalk were seen (Figures 1 A–C).
The diagnosis of hypothyroidism and hypercortisolism was made based on clinical presentation and laboratory investigations. After hormone replacement therapy, transsphenoidal excision of the suspected “pituitary macroadenoma” was performed in March 2019. An endoscopic approach via a unilateral nostril-sphenoidal route was used. During the procedure, a significant amount of thick yellowish-white pus was drained from the sellar region. There was no cerebrospinal fluid leakage during the operation. The cavity was fully cleaned and flushed with antibiotics and saline. Histopathology examination suggested an inflammatory lesion, possibly an abscess, with no evidence of pituitary adenoma. Broad-spectrum antibiotic therapy was administered for 2 weeks. The patient’s anemic status improved without the need for transfusion. Follow-up brain MRIs at 3 months and 1 year postoperatively showed that the lesion had resolved with no recurrence. The blood cell counts and endocrine test results were normal without the need for hormone replacement therapy. The patient developed temporary central diabetes insipidus, requiring oral desmopressin acetate for 1 year, and type 2 diabetes, controlled with medications.
A 38-year-old woman was referred to our neurosurgery department with complaints of gradually worsening throbbing headaches localized in the frontal region for about 2 months and blurry vision in the left eye for 2 weeks. She had no history of fever, polyuria, polydipsia, type 2 diabetes, sexual dysfunction, dysmenorrhea, or galactorrhea. She had irregular menstruation with minimal bleeding. Her husband had recently died in an accident, which led to prolonged insomnia and emotional distress.
The patient’s temperature was 36.8°C, and her blood pressure was 120/70 mmHg. She showed no signs of systemic infection or endocrine dysfunction other than those related to the pituitary.
Laboratory findings: Central hypothyroidism (free T4: 0.98 pmol/l, TSH: 3.62 mIU/l), elevated prolactin (95.8 ng/ml), low free testosterone (30.3 pmol/l), normal total cortisol (9.18 nmol/l), and nearly normal FSH and LH levels. The detailed information about the laboratory findings is shown in Table II.
Table II
Laboratory findings for case 2
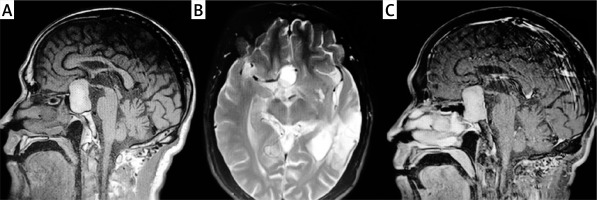
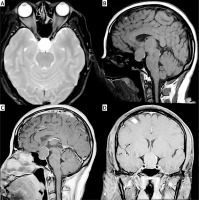
Brain MRI showed a capsulated solid mass in the sellar and suprasellar regions measuring 3.0 × 1.8 × 1.9 cm with peripheral enhancement. Gadolinium injection showed ring enhancement, and T2-weighted images indicated fluid within the lesion. The mass elevated the optic chiasm (Figures 2 A–D).
Endoscopic trans-sino-nasal-sphenoidal resection of the lesion was performed in April 2019. A significant amount of yellowish-white pus was drained during the surgery. Postoperatively, the patient’s headache disappeared, and her menstruation became regular. Follow-up MRI at 6 months showed that the pituitary stalk had thickened, and there were no more enhancing residual abscesses in the pituitary fossa, indicating complete resolution. Two years post-surgery, the patient had slightly weak but otherwise normal vision, and her menstrual volume increased without urorrhagia. Urinalysis and endocrine investigations showed normal results.
Pituitary abscess (PA) is a rare and serious condition with significant diagnostic challenges due to its nonspecific clinical presentation. Common symptoms include headache, visual disturbances, and hypopituitarism. Agyei et al. [3] reported that headache and visual disturbance are the most common complaints, occurring in 76.5% and 53.5% of patients, respectively. Similarly, Wang et al. [4] found that pituitary hypofunction and headache were the predominant symptoms in their series. In our cases, the patients presented with a combination of these symptoms, highlighting the importance of considering PA in the differential diagnosis of sellar masses.
MRI is crucial for the diagnosis of PA, though its findings often mimic other sellar lesions such as pituitary adenomas [1]. Typical MRI features include a mass with hypointense signals on T1-weighted images and hyperintense signals on T2-weighted images, often with rim enhancement following gadolinium administration. Our patients exhibited these MRI characteristics, reinforcing the need for high suspicion and careful radiological assessment.
Surgical intervention, particularly endoscopic transsphenoidal surgery, is considered necessary in most cases of PA. This approach offers minimal invasiveness, allowing effective drainage of the abscess with lower complication rates compared to craniotomy. Cabuk et al. [5] noted that transsphenoidal surgery had a lower recurrence rate of PA compared to craniotomy. Our cases demonstrate the efficacy of this surgical approach as both patients had successful outcomes with no recurrence.
Postoperative antibiotic therapy is essential to prevent infection recurrence, though cultures are often sterile due to prior antibiotic use or the difficulty in culturing certain pathogens. Liu et al. [6] reported that prolonged antibiotic therapy (3–6 weeks) is beneficial for PA patients. In our cases, a 2-week course of antibiotics was sufficient for recovery, suggesting that the duration of antibiotic therapy may need to be individualized based on clinical response and follow-up findings.
The 2 cases presented in this report highlight several important clinical insights:
Diagnostic challenges: Both cases underscore the diagnostic difficulties associated with PA. Despite typical clinical presentations and MRI findings, initial misdiagnosis as pituitary macroadenomas occurred. These cases emphasize the importance of maintaining a high index of suspicion for PA in patients with sellar masses and suggest that PA should be considered more readily when typical imaging features and clinical symptoms coexist.
Effective management: The successful treatment of both cases with endoscopic transsphenoidal surgery followed by a relatively short course of antibiotics demonstrates the effectiveness of this approach. This is consistent with the existing literature but also highlights the potential for individualized treatment duration based on patient response and follow-up findings.
Clinical outcomes: Both patients recovered without the need for long-term hormone replacement therapy, which is significant given that hypopituitarism is a common complication of PA. These cases suggest that prompt surgical intervention can preserve pituitary function and lead to favorable long-term outcomes.
In conclusion, PA is a rare condition that poses significant diagnostic and therapeutic challenges. The cases presented in this report demonstrate the importance of considering PA in the differential diagnosis of sellar masses and highlight the efficacy of endoscopic transsphenoidal surgery combined with antibiotic therapy. Early diagnosis and intervention are crucial for favorable outcomes. Further studies are needed to refine diagnostic criteria and optimize treatment protocols for PA.