Laryngeal cancer is a more common type of disease in the clinical otolaryngology department, and it is generally treated with surgical resection [1, 2]. Laryngeal cancer is the most common malignant tumors of head and neck in our country. The incidence is about 1.12/100 000 and the standardized death rate is 0.61/100 000 [3, 4]. Surgery for laryngeal cancer requires as much laryngeal function as possible while undergoing removal of the lesion [5]. There are different surgical methods for different stages of laryngeal cancer. The choice of surgical procedure is based on tumor size, location, possible post-operative dysfunction, surgical or radiation physician’s treatment level and experience, occurrence function, quality of life, and treatment outcome [6–8]. For T1-2N0 laryngeal cancer patients, oral laser resection of laryngeal cancer and oral robotic surgery are the most common options. Both of them have the characteristics of little trauma, no incision on the body surface, short hospital stay, low cost, and good functional recovery after surgery [9, 10]. For laryngeal cancer patients with T1-2N1-3/T3N0-3, surgery with or without radiotherapy or radiotherapy with cisplatin is recommended first if the patient can tolerate both surgery and cisplatin. Surgery is preferred for patients who can tolerate surgery but are intolerant to cisplatin. For patients who cannot tolerate surgery and can tolerate cisplatin, radiotherapy with cisplatin chemotherapy is preferred. For patients who cannot tolerate both surgery and cisplatin, radiotherapy alone is preferred [11]. For laryngeal cancer with a locally advanced stage or distant metastasis, an appropriate radiotherapy program can be selected according to lymph node involvement, major vessel involvement, incisal margin status, etc. [12].
In traditional surgical treatment, total larynx resection postoperative patients lose laryngeal function, are prone to swallowing disorders, and poor quality of life [13]. With the continuous development of surgical techniques, the emergence of partial laryngectomy makes it possible to preserve laryngeal function in patients with laryngeal cancer [14]. Partial laryngectomy currently includes horizontal partial laryngectomy and vertical partial laryngectomy. Both surgical methods are ideal in treating laryngeal cancer, and there is no unified clinical standard for which surgical treatment is taken, and the difference between the two surgical procedures is rarely reported [15]. To further determine the impact of the two surgeries on laryngeal cancer patients, this paper retrospectively analyzes the data of patients treated by the two surgeries in our hospital, analyzes the impact of the two surgeries on the quality of life and swallowing function. It is hoped that this study provides a theoretical basis for the clinical treatment of laryngeal cancer.
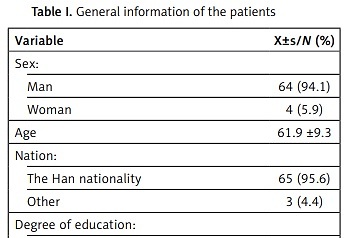
General data of 68 patients with glottic laryngeal squamous cell carcinoma admitted to our hospital between January 2020 and December 2021 were also retrospectively included. General information of the selected objects is shown in Table I.
Table I
General information of the patients
Inclusion criteria: (1) patients with first onset and first surgical treatment; (2) patients with preoperative pathological biopsy suggesting glottic laryngeal squamous cell carcinoma; (3) all patients underwent preoperative imaging examination to determine the primary lesion and the scope of invasion, without distant metastases; and (4) patients with complete clinical data. Exclusion criteria: (1) patients treated with chemoradiotherapy before surgery; (2) patients complicated with other malignancies; (3) patients with congenital laryngeal malformations; (4) patients with a history of laryngeal surgery; and (5) patients participating in other researchers. The prevalence of all subjects is shown in Table I.
According to the patient surgical procedure, only patients with simple vertical partial laryngeal resection or simple partial vertical laryngectomy were included, and 5 partial horizontal vertical laryngectomies and patients with metastases were excluded, and 63 patients were finally included as the study subjects.
The patient was intubated with a low endotracheal tube after local anesthesia. The curved transverse incision was centered on the ring methyl membrane, and the skin and the flap were separated layer by layer, and the white neck line was cut to fully expose the larynx. The annular cartilage cut the ring nail membrane to the vocal cord process and examined the glottis. The split carformate cartilage was detected in the median deviation, and the larynx was explored. After splitting the formoid cartilage, the affected formoid cartilage endoperiosteum should be peeled off, and the upper edge of the ventricular zone should be cut horizontally along the upper edge of the formoid cartilage toward the arytenoid epiglottitis. The upper and lower incision is combined, if necessary, and the arytenoid cartilage can be excised. The glottic defect was repaired in the pyriform fossa mucosa. The anterior residual edge of the lateral ventricular band and the vocal cord and the medial edge of the lateral ribbon muscle with the fascia band, bypassing the anterior counter-suture edge of the formoid cartilage plate, and stretching the anterior and posterior diameter of the throat. A notch at the upper end and the lower end of the thyroid cartilage plate was fixed, the anterior cervical ribbon muscle was strengthened, the drainage skin piece was placed, and the subcutaneous tissue was stitched in the opposite position.
After tracheotomy under local anesthesia, intubation, and general anesthesia, with a horizontal arc incision in the neck, the median lowest point was located in the middle of the parathyroid cartilage, at both ends of the leading edge of the sternocleidomastoid muscle. The latissimus neck flap was isolated and the hyoid and formoid cartilage were exposed. The superior hyoid muscle group on the upper side of the hyoid was cut close to the lesion, and cut in the middle of the hyoid or biased to the healthy side of the hypus on the affected side, which fully exposed the formoid cartilage. The hydromandrium was cut along the upper margin of the thyroid cartilage and dissected down, and the subpharyngeal constrictor attached to the lateral margin of the thyroid cartilage was severed, fully exposing the working thyroid cartilage. The inner periosteum was dissected, the upper half and upper angle of the affected parathyroid cartilage were removed, and the incision was slightly tilted up to avoid injuring the anterior combination. When cutting to the contralateral side, it was gradually tilted from the midline to retain the upper thyroid cartilage angle at the contralateral side. Cut the piriform nest on the affected side, the scissors toward the direction of the tongue will be wrinkled, cut to between the epiglottis and the root of the tongue for the whole layer cut, cut to the countermeasure tongue will be wrinkled. Observe the tumor range and wrinkle into the laryngeal vestibule in the contralateral laryngeal element, cut horizontally along the laryngeal chamber, separate the detection chamber and the vocal cord to the anterior combination, cut horizontally from the anterior to the posterior chamber in the affected laryngeal chamber, and remove the compartment above the vocal cord process to remove the specimen. When both sides of the arytenoid wrinkle into the laryngeal chamber, damage to the arytenoid cartilage should be avoided. Closing the arytenoid will wrinkle the mucosa and repair the residual medial mucosa and vocal cord margin of the piriform socket. The affected lateral hyoid was removed, the hyoid and formoid cartilage margin were closed with line 4, the hypopharyngeal mucosa was layered with suture, and the ribbon muscle was strengthened. The skin patch was drained, and the skin was sutured.
Total quality and dimension score levels of 2, 4, 12, 24, and 48 weeks, including distress, feeding process, swallowing symptom frequency, food choice, verbal communication, swallowing fear, panic, mental health, social life, fatigue and sleep frequency, and food texture, were observed. The correlation of the total quality of life (QoL) score with each dimension score was analyzed. The swallowing function classification was observed at different time points, and the correlation between swallowing function grade and quality of life was analyzed.
Using SPSS 23.0 statistical software, measurement data were represented as ± s, t-test, count data as percentage, using χ2 test, the contrast between multiple groups was detected by repeated measure variance, and p < 0.05 was considered statistically significant.
The swallowing QOL scores varied at different time points (p < 0.001); no significant difference between time and group interaction (p > 0.05) was observed; and the total swallowing QOL score between different groups is significant difference (p < 0.05) (Table II).
Table II
Comparison of the two surgical swallowing-related total scores of QoL
Statistical differences occurred at different time points (p < 0.001); no significant difference between time and group interaction was observed (p > 0.05); and distress scores between different groups are significant difference (p < 0.01) (Table III).
Table III
Comparison of the two types of postoperative distress-related QoL scores
In recent years, with the change of people’s lifestyle and eating habits and the aggravation of environmental pollution, the incidence of throat cancer has increased year by year. Clinical treatment of laryngeal cancer is mainly to improve the local control rate, preoperative evaluation of tumor scope, intraoperative protection of the cricoarytenoid joint, and postoperative swallowing function [6, 7]. At present, clinical partial laryngectomy is used to treat laryngeal cancer patients and good results are achieved [8, 9]. With the early detection of laryngeal cancer, the strengthening of the comprehensive treatment concept and the progress of repair and reconstruction means, laryngeal cancer surgery emphasizes the preservation of the laryngeal function as much as possible to improve the quality of life of patients [10, 11]. Therefore, how to choose surgical methods to improve the postoperative quality of life of patients has become the focus of clinical attention [12].
This paper retrospectively analyzes the clinical data of patients with glottic laryngeal squamous cell carcinoma in our hospital, compares the postoperative quality of life of patients with partial and horizontal laryngectomy, the results of two kinds of patients are better/different at different time points than patients at different time points, suggesting that the postoperative quality of life of patients treated by vertical partial resection is better. The comparison of the scores of the other dimensions of the quality of life also showed that the vertical hemithroat patients were significantly better than those of the other dimensions. The swallowing function of both surgical patients was also graded later, and the results showed that the swallowing function grade was also significantly different between the two groups. This was because the partial horizontal laryngectomy was performed above the level of the vocal cord, the complete removal of the supraglottic structure, the normal movement of the lateral arytenoid cartilage, and the vocal cord was retained intact [1]. However, with the loss of laryngeal vestibular structure, the protective function of the larynx was completely compensated by the glottis closure, and the chance of vocal cord mucosal impact was increased, resulting in mucosal thickening and affecting the swallowing function and quality of life [3]. However, vertical laryngeal partial resection can retain the normal swallowing and occurrence of the function to the greatest extent, due to the more preserved tissue, the postoperative swallowing function and quality of life of patients are not affected [13]. When observing the relationship between swallowing function grade and QOL, it was found that the two groups of surgical patients were mostly negatively correlated with the total score of quality of life, indicating that the higher the QOL score, the lower the swallowing function grade, and the better the swallowing function. This paper compares the quality of life and swallowing function in the patients of the two different surgical methods, and thus provides a basis for the clinical treatment of laryngeal cancer. This will provide more reference for the selection of laryngeal cancer surgery.
However, this paper still has some limitations: (1) Small sample size. Only 63 patients were included in this study; (2) The comparison between primary outcome indicators and secondary outcome indicators is not clear so it is difficult to draw an accurate and complete clinical conclusion; (3) The evaluation system is relatively simple, and more authoritative and comprehensive scales can be further adopted to evaluate it in the follow-up process. The next step will be a multicenter large-sample control study to further verify the accuracy of the results.
In conclusion, vertical partial laryngectomy for patients with glottic laryngeal squamous cell carcinoma is helpful to improve the postoperative quality of life and significantly improve the swallowing function, which is worthy of clinical application and promotion.