Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
Early prediction of placenta accreta spectrum by evaluation of risk factors and ultrasound
1
Department of Obstetrics, Xiangya Hospital Central South University, Changsha, China
2
Hunan Engineering Research Center of Early Life Development and Disease Prevention, Changsha, China
3
Reproductive Medicine Center, Xiangya Hospital Central South University, Changsha, China
Submission date: 2023-10-11
Final revision date: 2023-11-23
Acceptance date: 2023-12-09
Online publication date: 2024-10-31
Corresponding author
Jingrui Huang
Department of Obstetrics, Xiangya Hospital, Central South University, 87 Xiangya Road, Changsha 410008, China
Department of Obstetrics, Xiangya Hospital, Central South University, 87 Xiangya Road, Changsha 410008, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
We explored the predictive utility of clinical risk factors and first-trimester pregnancy ultrasound signs for severe placenta accreta spectrum.
Material and methods:
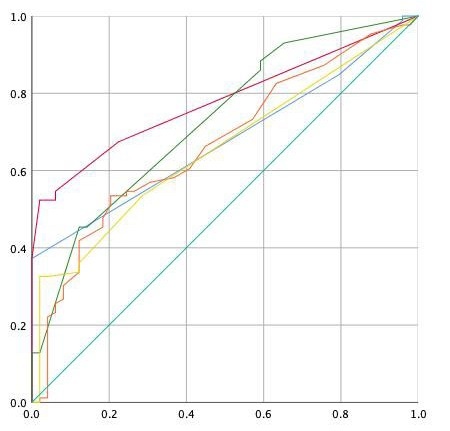
Patients with placenta accreta spectrum treated in our institution between March 1, 2017 and December 31, 2022 were analyzed. The patients were divided into those with mild and those with severe conditions. Univariate analysis was used to determine the clinical risk factors and first trimester ultrasound signs associated with severe placenta accreta spectrum. Receiver operating characteristic curves were drawn and the areas under the curves calculated.
Results:
Univariate analysis revealed significant between-group differences between the groups in the number of cesarean sections, scar pregnancy, low gestational sac position, abnormal placental position, focal exophytic mass and abnormal placental lacunae in placental parenchyma (p < 0.05). The number of cesarean sections and first trimester ultrasound signs predicted severe placenta accreta spectrum, with areas under the curves of 0.66 and 0.75. When the number of cesarean sections was combined with low gestational sac position, the placenta position and related ultrasound signs, the areas under the curves for predicting severe placenta accreta spectrum were 0.78, 0.73, and 0.89, respectively.
Conclusions:
Clinical risk factors and first-trimester ultrasound signs predicted severe placental accreta spectrum and their combinations had even greater clinical utility.
We explored the predictive utility of clinical risk factors and first-trimester pregnancy ultrasound signs for severe placenta accreta spectrum.
Material and methods:
Patients with placenta accreta spectrum treated in our institution between March 1, 2017 and December 31, 2022 were analyzed. The patients were divided into those with mild and those with severe conditions. Univariate analysis was used to determine the clinical risk factors and first trimester ultrasound signs associated with severe placenta accreta spectrum. Receiver operating characteristic curves were drawn and the areas under the curves calculated.
Results:
Univariate analysis revealed significant between-group differences between the groups in the number of cesarean sections, scar pregnancy, low gestational sac position, abnormal placental position, focal exophytic mass and abnormal placental lacunae in placental parenchyma (p < 0.05). The number of cesarean sections and first trimester ultrasound signs predicted severe placenta accreta spectrum, with areas under the curves of 0.66 and 0.75. When the number of cesarean sections was combined with low gestational sac position, the placenta position and related ultrasound signs, the areas under the curves for predicting severe placenta accreta spectrum were 0.78, 0.73, and 0.89, respectively.
Conclusions:
Clinical risk factors and first-trimester ultrasound signs predicted severe placental accreta spectrum and their combinations had even greater clinical utility.
REFERENCES (28)
1.
Einerson BD, Gilner JB, Zuckerwise LC. Placenta accreta spectrum. Obstet Gynecol 2023; 142: 31-50.
2.
Jauniaux E, Ayres-de-Campos D, Langhoff-Roos J, et al. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO classification for the clinical diagnosis of placenta accreta spectrum disorders. Int. J Gynaecol Obstet 2019; 146: 20-4.
3.
Jauniaux E, Ayres-de-Campos D. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: introduction. Int J Gynaecol Obstet 2018; 140: 261-4.
4.
Obstetrics Group of Obstetrics and Gynecology Branch of Chinese Medical Association, Maternal and Fetal Medicine Special Committee of Obstetrics and Gynecology Branch of Chinese Medical Doctor Association. Guidelines for the diagnosis and management of placenta accreta spectrum (2023). Chinese J Perinatal Med 2023; 26: 617-27.
5.
Hong S, Le Y, Lio KU, Zhang T, Zhang Y, Zhang N. Performance comparison of ultrasonography and magnetic resonance imaging in their diagnostic accuracy of placenta accreta spectrum disorders: a systematic review and meta-analysis. Insights Imaging 2022; 13: 50.
6.
Shainker SA, Coleman B, Timor-Tritsch IE, et al. Society for Maternal-Fetal Medicine. Electronic address: pubs@smfm.org. Special Report of the Society for Maternal-Fetal Medicine Placenta Accreta Spectrum Ultrasound Marker Task Force: Consensus on definition of markers and approach to the ultrasound examination in pregnancies at risk for placenta accreta spectrum. Am J Obstet Gynecol 2021; 224: B2-14.
7.
Zheng W, Zhang H, Ma J, et al. Validation of a scoring system for prediction of obstetric complications in placenta accreta spectrum disorders. J Matern Fetal Neonatal Med 2022; 35: 4149-55.
8.
D’Antonio F, Calagna G, Sara T, Gaspare C, Chiantera V, Calì G. Abnormal placenta implantation. Integration between first- and third-trimester imaging in predicting the severity of Placenta Accreta Spectrum (PAS) disorders. J Clin Ultrasound 2023; 51: 311-7.
9.
Sentilhes L, Kayem G, Chandraharan E, Palacios-Jaraquemada J, Jauniaux E. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: Conservative management. Int J Gynaecol Obstet 2018; 140: 291-8.
10.
Carusi DA. The placenta accreta spectrum: epidemiology and risk factors. Clin Obstet Gynecol 2018; 61: 733-42.
11.
Guo Z, Ma J, Yang H. Is twin gestation an independent risk factor for placenta accreta spectrum? Am J Obstet Gynecol 2022; 226: 446-7.
12.
Arakaza A, Zou L, Zhu J. Placenta accreta spectrum diagnosis challenges and controversies in current obstetrics: a review. Int J Womens Health 2023; 15: 635-54.
13.
Khander A, Sharma N, Eroglu I, Chasen ST. Ultrasound detection rates of the placenta accreta spectrum with prior myomectomy. J Matern Fetal Neonatal Med 2022; 35: 8752-5.
14.
Romeo V, Verde F, Sarno L, et al. Prediction of placenta accreta spectrum in patients with placenta previa using clinical risk factors, ultrasound and magnetic resonance imaging findings. Radiol Med 2021; 126: 1216-25.
15.
Jauniaux E, Chantraine F, Silver RM, Langhoff-Roos J. FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: epidemiology. Int J Gynaecol Obstet 2018; 140: 265-73.
16.
Szymusik I, Kosinska-Kaczynska K, Krowicka M, Sep M, Marianowski P, Wielgos M. Perinatal outcome of in vitro fertilization singletons – 10 years’ experience of one center. Arch Med Sci 2019; 15: 666-72.
17.
Günay T, Yardımcı OD. How does subchorionic hematoma in the first trimester affect pregnancy outcomes? Arch Med Sci 2021; 18: 639-46.
18.
Tovbin J, Melcer Y, Shor S, et al. Prediction of morbidly adherent placenta using a scoring system. Ultrasound Obstet Gynecol 2016; 48: 504-10.
19.
Happe SK, Yule CS, Spong CY, et al. Predicting placenta accreta spectrum: validation of the placenta accreta index. J Ultrasound Med 2021; 40: 1523-32.
20.
Pekar-Zlotin M, Maymon R, Eliassi Revivo P, et al. Comparison between a prenatal sonographic scoring system and a clinical grading at delivery for placenta accreta spectrum disorders. J Matern Fetal Neonatal Med 2022; 35: 8810-6.
21.
Doulaveris G, Ryken K, Papathomas D, et al. Early prediction of placenta accreta spectrum in women with prior cesarean delivery using transvaginal ultrasound at 11 to 14 weeks. Am J Obstet Gynecol MFM 2020; 2: 100183.
22.
Calí G, Timor-Tritsch IE, Forlani F, et al. Value of first-trimester ultrasound in prediction of third-trimester sonographic stage of placenta accreta spectrum disorder and surgical outcome. Ultrasound Obstet Gynecol 2020; 55: 450-9.
23.
Yu FNY, Leung KY. Antenatal diagnosis of placenta accreta spectrum (PAS) disorders. Best Pract Res Clin Obstet Gynaecol 2021; 72: 13-24.
24.
Guzmán López JA, Gutiérrez Sánchez LÁ, Pinilla-Monsalve GD, Timor-Tritsch IE. Placenta accreta spectrum disorders in the first trimester: a systematic review. J Obstet Gynaecol 2022; 42: 1703-10.
25.
Marsoosi V, Ghotbizadeh F, Hashemi N, Molaei B. Development of a scoring system for prediction of placenta accreta and determine the accuracy of its results. J Matern Fetal Neonatal Med 2020; 33: 1824-30.
26.
Abu Hashim H, Shalaby EM, Hussien MH, El Rakhawy. Diagnostic accuracy of the placenta accreta index for placenta accreta spectrum: a prospective study. Int J Gynaecol Obstet 2022; 156: 71-6.
27.
Ming Y, Zeng X, Zheng T, Luo Q, Zhang J, Zhang L. Epidemiology of placenta accreta spectrum disorders in Chinese pregnant women: a multicenter hospital-based study. Placenta 2022; 126: 133-9.
28.
Yang X, Zheng W, Yan J, Yang H. High risk factors for placenta accreta other than pregnancy and their impact on patient prognosis. Matern Fetal Med 2023; 5: 137-43.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.