Chronic pancreatitis (CP) is a common disease that presents with fibrosis and dysfunction of the endocrine and exocrine glands of the pancreas [1]. The etiology of CP is complicated. Recurrent acute pancreatitis (RAP) is defined as ≥ 2 episodes of AP and is an important risk factor for CP, as confirmed by a large number of clinical studies [2]. However, not all patients with RAP develop to CP [3]. A meta-analysis showed that nearly 70% of RAP patients did not progress to CP [4]. Identifying risk factors for progression of RAP to CP is important because it could facilitate earlier intervention and may potentially delay or avoid the onset of CP, although there were some drugs that might delay CP progression [5]. To evaluate the risk factors of patients with RAP progression to CP, we designed a retrospective study involving a cohort of 265 patients with RAP.
Methods
We retrospectively retrieved the medical information of patients with RAP between January 2012 and December 2019, in the Department of Gastroenterology of Peking University Third Hospital. The study protocol was approved by the Human Ethics Review Committees of Peking University Third Hospital (No: M2019402). As a retrospective study, the ethics committee waived the need for written informed consent. Inclusion criteria were as follows: 1) Patients experienced at least 2 acute AP episodes before CP diagnosis. 2) The AP diagnosis was based on the revision of the Atlanta classification [6]. 3) All patients were evaluated for clinical diagnosis of chronic pancreatitis according to the M-ANNHEIM diagnostic criteria [7] and only patients with no signs of CP were included. Exclusion criteria were: < 18 years of age, autoimmune pancreatitis, mass within the pancreatic head, pancreatic cancer and patients who lacked imaging data of the pancreas which could prove the diagnosis of CP or not during follow-up. The etiology of AP was defined according to previous guideline [8]. All patients were evaluated for clinical diagnosis of chronic pancreatitis and underwent computed tomography (CT) scan, magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangio-pancreatography (ERCP) at each AP episode during follow-up and were diagnosed with defined CP according to the M-ANNHEIM diagnostic criteria [7]. SPSS 25.0 and R software (version 3.2.4) were used for data analysis. The nomogram scaled each regression coefficient to a scale of 0–100 points, which demonstrated their relative importance. Based on the total score from the nomogram, the optimal cutoff value was identified by X-tile software and patients were divided into two risk groups (low- and high-risk). Statistical significance was set at p < 0.05.
Results
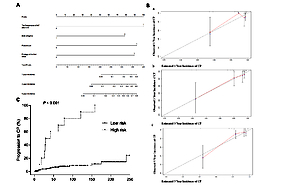
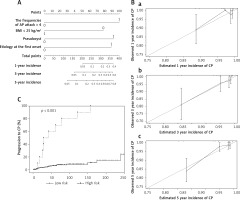
A total of 265 patients diagnosed with RAP were included in our study. The patients’ baseline characteristics are listed in Table I. During the follow-up, a total of 29 patients were diagnosed with CP. The median duration from the first onset of AP to the diagnosis of CP was 33 months (interquartile range: 10–57.5 months). Univariate analysis indicated that the risk factors for progression from RAP to CP included the severity and etiology at the first onset, number of RAP episodes, chronic pain, presence of pseudocysts, and body mass index (BMI) < 25 kg/m2. In multivariate analysis, we divided the etiology of patients at the first onset into idiopathic and non-idiopathic. Multivariate analysis revealed that the risk factors of progression from RAP to CP were the number of RAP episodes, presence of pseudocysts, idiopathic pancreatitis and BMI < 25 kg/m2 (Table II). Four independent predictors were used to develop a risk estimation nomogram for RAP progression to CP (Figure 1 A). The nomogram demonstrated good accuracy in estimating the risk of CP, with a C-index of 0.817 (95% CI: 0.72–0.91). The calibration curves showed good consistency between risk estimates through the nomogram and actual development of CP at 3 and 5 years after patients were admitted (Figure 1 B). The nomogram score of 192.2 points was the optimal cutoff value through the X-tile analysis. Patients were divided into a low-risk group (≤ 192.2 points) and a high-risk group (> 192.2 points) according to the nomogram prediction score. The Kaplan-Meier curve showed that the risk of progression to CP in the high-risk group was significantly higher than that in the low-risk group (p < 0.001) (Figure 1 C).
Table I
General characteristics of all 265 patients
| Items | Total (n = 265) n (%) | RAP (n = 236) n (%) | RAP-CP (n = 29) n (%) | P-value |
|---|---|---|---|---|
| Female (%) | 96 (36.2) | 90 (38.1) | 6 (20.7) | 0.065 |
| BMI [kg/m2]: | 0.005 | |||
| < 25 | 155 (58.5) | 131 (55.5) | 24 (82.8) | |
| ≥ 25 | 110 (41.5) | 105 (44.5) | 5 (17.2) | |
| Age at CP diagnosis [years] | 42 (33–53) | 41 (33–46) | 43 (32–55) | 0.148 |
| Follow-up time [months] | 38 (11.3–73.8) | 74.5 (39–122) | 33 (10–57.5) | 0.185 |
| Drinking history [years] | 20 (10–30) | 20 (10–30) | 20 (10–30) | 0.222 |
| Smoking history [years] | 20 (10–30) | 20 (10–30) | 20 (10–30) | 0.344 |
| Severity at first onset (%): | < 0.001 | |||
| Mild | 225 (84.9) | 211 (89.4) | 14 (48.3) | |
| Moderate | 20 (7.5) | 12 (5.1) | 8 (27.6) | |
| Severe | 20 (7.5) | 13 (5.5) | 7 (24.1) | |
| Etiology of first onset (%): | < 0.001 | |||
| Biliary | 87 (32.8) | 85 (36.0) | 2 (6.9) | 0.001 |
| Alcoholic | 38 (14.3) | 35 (14.8) | 3 (10.3) | 0.374* |
| Idiopathic | 119 (44.9) | 95 (40.3) | 24 (82.8) | < 0.001 |
| Other known causes | 21 (7.9) | 21 (8.9) | 0 (0) | 0.079* |
| Clinical characteristics: | ||||
| Episodes of AP attack | 3 (2–4) | 5 (4–8) | 3 (2–4) | 0.019 |
| Cholecystectomy (%) | 42 (15.8) | 41 (17.4) | 1 (3.4) | 0.059 |
| Chronic pain (%) | 7 (2.6) | 4 (1.7) | 3 (10.3) | 0.031 |
| Pseudocyst (%) | 40 (15.1) | 26 (11.0) | 14 (48.3) | < 0.001 |
Table II
Predictive factors for RAP progression to CP
Figure 1
A – Nomogram for recurrent acute pancreatitis progression to chronic pancreatitis. B – Effectiveness of predictive performance of the nomogram in estimating the risk of CP. (a) 1-year incidence in the RAP cohort; (b) 3-year incidence in the RAP cohort; (c) 5-year incidence in the RAP cohort. The validity of the nomogram showed that the predictive value of progression to CP at 3 and 5 years is better than that at 1 year. This is consistent with our knowledge, as RAP often takes some time to progress to CP. C – Rate of progression to CP after a first attack of acute pancreatitis according to the hazard stratification (Kaplan-Meier curve and one minus survival)
Discussion
There are some important findings of our study. First, we found that more than 4 episodes of RAP, idiopathic pancreatitis, BMI < 25 kg/m2 and pseudocysts were independent risk factors for progression to CP. Second, we developed a simple tool to help clinicians early identify high-risk RAP patients who might progress to CP. Our results revealed that patients who experienced more than 4 episodes of AP had a higher risk of progression to CP (HR = 3.816, 95% CI: 1.655–8.797), which was consistent with Péter J. Hegyi’s study [9].Their study also found that the pancreas of the mice could develop chronic pancreatitis-like changes if there were more than three episodes of RAP. And for patients with more than three RAP episodes, the total pancreatic volume decreased significantly, although there were no clinically common manifestations of CP [10]. Idiopathic pancreatitis is one of the risk factors for RAP progression to CP in our study and exhibited a higher rate of progression to CP. Idiopathic pancreatitis also often leads to an increased risk of progression to CP by a higher recurrent rate due to the lack of targeted treatment [11]. On the other hand, genetic factors might participate in and accelerate the procession of developing CP, such as SPINK1p.N34S in European patients and PRSS1 mutation in Chinese patients [11, 12]. These mutations could help us understand why the rate of progression to CP is so high in patients with idiopathic pancreatitis.
In our study, pancreatic pseudocysts were another independent risk factor for RAP progression to CP. All patients underwent evaluation of clinical diagnosis of CP when they were included in the cohort, so pseudocysts could not be the manifestation of CP. The incidence of pseudocysts increased significantly in patients with CP, which might be associated with pancreatic duct stones, protein embolism, and local fibrosis [13]. Although there have been no studies that described in detail the role of pseudocysts in RAP progression to CP, given the above mechanisms, we speculate that pseudocysts might lead to pancreatic duct damage and morphological changes. Patients with CP often lose weight due to pancreatic exocrine insufficiency, poor fat absorption and recurrent pain [14]. In the present study, BMI < 25 kg/m2 was another risk factor for RAP progression to CP. Like the role of pseudocysts for progression to CP, lower BMI was not a manifestation of CP but a risk factor. We have assessed all RAP patients with underweight or pseudocysts carefully according to the M-ANNHEIM diagnostic criteria to exclude potential early CP of these patients. Since early CP is difficult to diagnose at present, there may still be some bias in the current study, which requires further evidence from a prospective study in the future.
In conclusion, according to the nomogram, we developed a simple tool to help clinicians use it in outpatient clinics to divide RAP patients into high-risk and low-risk groups. Patients in the high-risk group are more likely to progress to CP and need active intervention or close follow-up.