Ectopic calcification is a pathological condition resulting from abnormal deposition of salt ions in the soft tissues of the body. There are several types of ectopic calcifications, including calciphylaxis, metastatic calcifications, nodular calcifications, idiopathic calcifications and dystrophic calcifications, the latter type being the subject of this paper [1]. This particular type of biomineral disorder is most often associated with a history of trauma, infection or infestation of the affected area, and it progresses without visible abnormalities in blood calcium levels [2]. In some cases, calcifying lesions may represent a local, non-specific response of unknown origin [3]. Dystrophic calcification can occur in any soft tissue, with the most prevalent location being the vascular and cardiac tissue, particularly often occupying a myocardial or valvular mass [4]. The lesions in head and neck tissues are extremely rare. They are asymptomatic, and the disease is diagnosed incidentally [5]. Based on the literature analysis, the case presented below represents the 6th described dystrophic masseter muscle calcification in the world.
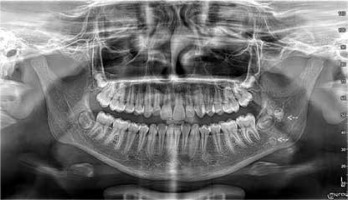
A 12-year-old female patient was admitted to the Clinical Department of Maxillofacial Surgery at the 4th Military Clinical Hospital in Wroclaw for biopsy of the left mandibular angle due to an interstitial lesion of the left masseter muscle, which had been discovered several months earlier. On palpation, lesions were perceptible from external and internal access in the form of two associated nodules, superficially and deeply located in relation to each other. The lesion was non-painful, hard, movable relative to the unchanged skin. Activity and function of nerves V and VII and Stensen’s ducts were bilaterally normal. The ultrasound image revealed two well-demarcated hyperechoic lesions measuring approx. 8 × 6 mm and 4 × 4 mm with an acoustic shadow visible below. The lesion was located within the masseter muscle, slightly forward of the anterior margin of the parotid gland. The image suggested calcification/stone (Figure 1). Orthopanthomogram (OPG) and cone beam computed tomography (CBCT) scan revealed two highly saturated foci within the masseter muscle (Figures 2 and 3). In laboratory tests, no abnormalities in ionic and endocrine metabolism were observed, total calcium was at 2.65 mmol/l. It was decided to have an open biopsy of the nodules. The lesion was removed bluntly after dissection of the masseter muscle with access through the oral vestibule. The removed material was sent for histopathological examination, which described two lesions with diameters of 0.8 cm and 0.6 cm. Cross-sections showed fibrous tissue with foci of calcification and central necrosis (Figure 4). After excluding calcium disorders, a diagnosis indicating calcifications of the dystrophic type of the masseter muscle was made.
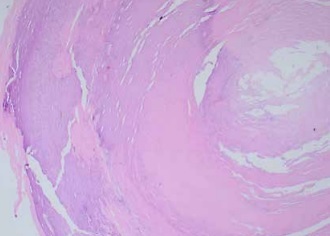
Figure 1
Ultrasound image of a well-demarcated hyperechoic lesion measuring 4x4 mm within the left masseter muscle (white arrow), MM – masseter muscle, M – mandible
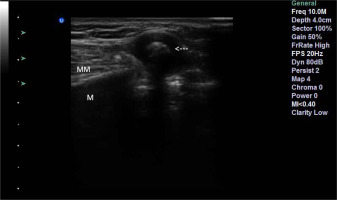
Figure 3
CBCT image showing two highly saturated lesions located near the left mandibular angle (white arrows)

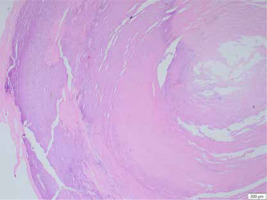
Figure 4
Cross-section showing fibrous tissue with foci of calcification (left side) around central necrosis (right side)
Based on the available English literature, the case presented here is the first report of dystrophic calcification in the masseter muscle in Central Europe and the second such condition reported in a female patient.
The pathomechanism of dystrophic calcification is characterized by the occurrence of soft tissue damage leading, through a series of phenomena, to the deposition of calcium salts within the tissue, including hydroxyapatite and amorphous calcium phosphate. This process takes place without any noticeable variation in the concentrations of the above elements in the blood. The dying cells within the lesion release phosphorus-binding proteins. High concentrations of calcium and phosphate are released in the mitochondria of cells, thus leading to crystal formation and cell necrosis. This process is further exacerbated by tumor necrosis factor (TNF), interleukin (IL) 6 (IL-6) and IL-1. This condition may be accompanied by chronic inflammation and vascular hypoxia [6].
The medical history of the 12-year-old patient we describe, admitted to the Clinical Department of Maxillofacial Surgery at the 4th Military Clinical Hospital in Wroclaw, did not indicate a history of infection or trauma to the affected area. Analyzing the case we present and the cases published in the literature collected in the table below, it is possible to notice a tendency for dystrophic calcification to appear in an area of soft tissue not covered by previous pathology. Thus, it can be concluded that the dystrophic changes described so far, differ in their nature from textbook features and only Kim et al. when describing the case of a 26-year-old woman, indicated a previous injury to the muscle in the patient’s 4th year of life [3]. However, it should be borne in mind that in many cases, the lack of information about past medical conditions may not reflect the facts of the patient’s history, particularly with regard to early childhood injuries.
In the light of the described case, special attention should be paid to the importance of appropriately selected diagnostics. A number of calcifying lesions can be located within the facial region, such as calcifying lymph nodes, dystrophic calcifications, venous malformations and neoplastic lesions [1]. The first step towards an accurate diagnosis should be to narrow down the range of possible diseases on the basis of imaging studies, supplemented by laboratory tests. The imaging study of choice in pediatric patients should be ultrasound. Due to the lower adipose tissue content in the head and neck region compared to the adult population, there is better tissue penetration by ultrasound in children, allowing for better resolution images to be obtained. The use of Doppler ultrasound also allows the vascularization of the lesion to be assessed. Ultrasound-based diagnostics allows an initial assessment of palpably detected pathology without exposing the patient to high doses of X-rays and without the need for sedation, often required for computed tomography (CT) or magnetic resonance imaging (MRI) scans in children [7]. Pediatric patients show particular sensitivity to the radiation used in CT scans, so it should be performed as an adjunct to ultrasound after assessing the need for expanded diagnostic imaging. It is important to remember the recommended reduction in radiation doses for children [8].
Presented to stomatology in 1998, CBCT has become an extremely helpful imaging test in the diagnosis of diseases located in the head and neck region [9]. This innovative maxillofacial imaging technique produces accurate, high-resolution images using doses much lower than those used in CT scans [10]. The examination results in a three-dimensional image of the dental structures and bones in the craniofacial region in a single scan, which enables more precise treatment planning. It is important to remember that the correct imaging modality, regardless of the age of the patient, is one that provides as much information as possible about the lesion in the safest way for the individual and as quickly as possible to perform.
Pediatric patients are significantly less likely to develop a malignant neoplastic lesion in the head and neck than the adult patient population [11]. However, this does not preclude the need for a biopsy to accurately assess the palpable soft tissue lesion. Cytological examination of a palpable lesion should be considered the gold standard and be the final step towards an accurate diagnosis. Fine needle aspiration (FNA) biopsy has a number of advantages, including being a quick and inexpensive procedure that does not require hospitalization, with a low risk of complications. For pediatric patients, however, sedation is often required during FNA so an open surgical biopsy may be a much better option here, not only providing material for histopathological examination but also forming a part of the treatment based on removal of the entire lesion.
As a consequence of the particular rarity of dystrophic calcification in head and neck tissues, there is no clear protocol for the treatment of the above condition. Reports of drug treatment include lesions of other regions, including the bladder and skin. In the above cases, it has been reported that smaller lesions respond to warfarin, ceftriaxone while larger lesions show sensitivity to diltiazem, bisphosphonates, probenecid and aluminum hydroxide [6, 12, 13]. Regardless of the size of the lesion, surgical removal of the calcification should also be considered, with factors such as size, location, age and general condition of the patient guiding the final decision. The surgical access to the lesion should be as small and subtle as possible in order to avoid additional potentially lesion causing trauma.
Analyzing the entirety of the presented case, we can undoubtedly state that dystrophic calcification is a discrete condition whose diagnosis relies on the vigilance of the patient or a skillful examining doctor, and in the area we have described – especially the dentist. Although calcification of the masseter muscle is not a serious pathology, it is important that, if a similar lesion is observed, a diagnosis is made as soon as possible to exclude other, more serious lesions. Due to the rarity of the condition, there are no long-term observation reports of cases without any surgical or pharmacological interventions. Therefore, it is difficult to determine further development without treatment.
In conclusion, dystrophic calcification of the masseter muscle is a rare lesion of head and neck tissues. Diagnostic success and correct treatment are based on imaging, laboratory blood tests and histopathological examination of the affected tissue.