As hepatic enzyme serum concentrations are associated with not only liver diseases but also obesity and type 2 diabetes in adults [1–3], early detection of laboratory parameter change is key for screening and prevention [4]. Although several approaches have been performed to establish solid and precise new reference intervals or thresholds for liver enzymes [5], their significance in the context of age and gender still requires validation. Furthermore, chronological changes in establishment of upper reference limits (URLs) have never been explored due to scarcity of data providing regular follow-up in liver enzymes in the apparently healthy population. Additionally, various age- and gender-related percentiles of liver enzymes have been suggested as the URLs in different ethnic populations [6].
Korea has systematic and comprehensive national registry data collected from the Korean National Health Insurance Service-National Sample Cohort (KNHIS-NSC) [7]. The KNHIS-NSC database is a population-based sample cohort. Its purpose is to provide representative, useful health insurance and health examination data to public health researchers and policymakers. A total of 1,025,340 participants (513,258 men and 512,082 women) participants were followed for 11 years, until 2013. Importantly, the data include not only laboratory results from general health examinations, but also information about participants’ insurance eligibility, medical treatment history, and healthcare providers’ institutions.
The purpose of this study was to investigate the gender differential chronological changes in URLs in healthy adult individuals in the KNHIS-NSC database using a nationwide, population-based, 11-year retrospective cohort.
Methods
Database and study population
Data for this study were derived from the database KNHIS-NSC 2002–2013. This database includes all medical claims and general health examination results filed from January 2002 to December 2013. The study population for this study comprised nationally representative subjects who have undertaken biannual medical check-ups in all three of the following periods: 2003–2004, 2007–2008, and 2012–2013. For diagnostic codes, the KNHIS uses the Korean Classification of Diseases (KCD), which is similar to the International Classification of Diseases (ICD). This study adhered to the tenets of the Declaration of Helsinki, and the KNHIS-NSC 2002–2013 project was approved by the Institutional Review Board of the KNHIS.
A flowchart for the study population is presented in Figure 1 A. From a total of 268,024 Koreans who participated in medical check-ups in all three periods (year 2002–2003, 2007–2008, and 2012–2013), we excluded subjects with a history of liver disease during the 11 years of the study period (n = 159,744) using the KNHIS-NSC 2002–2013 database. Among the 108,280 apparently healthy subjects, we excluded those missing liver enzyme variables that we examined in this study (n = 85). Then, we selected individuals who were between 40 years and 74 years old at the baseline. Thus, we analyzed a total of 107,999 individuals (61,189 men and 46,810 women). We further divided the study population into 14 subgroups according to age (interval 5 years) and gender. Group 1 was defined as subjects who were 40–44 years old in the first period (year 2002 or 2003), and group 2 was defined as subjects who were 45-49 years old in the first period, and so on until group 7.
Figure 1
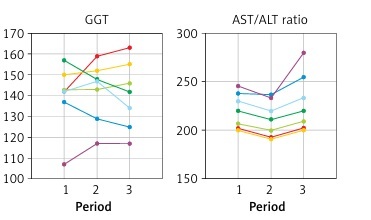
Overview and results of the study design. A – Flowchart of study population selection. B – Chronological changes of 97.5th upper reference limit values in ALT, AST, GGT, and AST/ALT ratio for 14 subgroups according to age and gender. Changes were evaluated during three periods with a time interval of 5 years. Group 1: 40–44 years old at the first period; Group 2: 45–49 years old; Group 3: 50–54 years old; Group 4: 55–59 years old; Group 5: 60–64 years old; Group 6: 65–69 years old; Group 7: 70–74 years old. Period 1: years 2002–2003; Period 2: years 2007–2008; Period 3: years 2012–2013

Definition of apparently healthy population
Each patient was tracked on the basis of his or her index dates for ambulatory and inpatient care visits over the 11 years from 2003 to 2013, to detect those patients who developed non-alcoholic fatty liver disease (NAFLD) (KCD code K76.0, corresponding to ICD-10-CM code K76.0). To rule out the effects of liver disease with other etiologies, we excluded subjects who also had a diagnosis of alcoholic fatty liver or toxic liver (KCD codes K70–75).
To confirm the health status of all subjects, we also reviewed self-reported medical questionnaires in all the subjects. Only individuals without any medical diagnosis were included in the study.
Liver enzyme variables
We chronologically compared serum ALT, AST, and GGT in all subjects in the 14 subgroups, calculating absolute differences of mean values for numerical parameters and percentage differences for liver enzyme parameters from 2002–2003 to 2007–2008 and from 2007–2008 to 2012–2013. Furthermore, AST/ALT ratio was calculated in each individual and investigated as another independent parameter. As the time intervals were both approximately 5 years, we could also compare changes between 2 time periods within each group.
Statistical analysis
A total of 4 percentiles were derived to be presented as possible URL values: 95th, 97.5th, 99th, and 99.5th percentiles. The differences among the 7 age subgroups were evaluated by ANOVA test. P-values < 0.05 were considered statistically significant. All analyses were conducted using SAS v9.4 (SAS Institute Inc., USA). Chronological trends were assessed by calculating absolute differences between adjacent periods, and unanimous directional changes were considered as the chronological trend direction.
Results
Upper reference limit values of ALT, AST, and GGT in 14 subgroup cohorts.
The URL values of ALT, AST, and GGT according to four different percentiles in the whole studied population are shown in Table I. Although all the mean values were higher in men than women, covariances (CV) were similar between men and women. When ratios among 3 high percentiles over the 95th percentile were compared between men and women, AST and GGT still showed greater incremental ratios in men compared to women.
Table I
Upper reference limit values of ALT, AST, and GGT using 4 different percentiles
| Parameter | ALT | AST | GGT | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | CV | Ratio* | Mean | SD | CV | Ratio* | Mean | SD | CV | Ratio* | |
| Men | ||||||||||||
| 95th percentile | 46.3 | 6.0 | 12.9% | 1.00 | 42.6 | 1.4 | 3.3% | 1.00 | 99.3 | 12.7 | 12.8% | 1.00 |
| 97.5th percentile | 57.2 | 8.1 | 14.1% | 1.24 | 50.9 | 2.1 | 4.2% | 1.20 | 140.7 | 14.8 | 10.5% | 1.42 |
| 99th percentile | 75.6 | 10.4 | 13.8% | 1.63 | 68.0 | 3.8 | 5.6% | 1.60 | 214.7 | 27.1 | 12.6% | 2.16 |
| 99.5th percentile | 93.3 | 14.2 | 15.2% | 2.02 | 86.6 | 8.8 | 10.1% | 2.03 | 291.4 | 41.0 | 14.1% | 2.94 |
| Women | ||||||||||||
| 95th percentile | 35.6 | 3.2 | 8.9% | 1.00 | 36.2 | 1.7 | 4.6% | 1.00 | 41.3 | 5.0 | 12.2% | 1.00 |
| 97.5t h percentile | 43.4 | 4.2 | 9.8% | 1.22 | 42.2 | 2.4 | 5.6% | 1.17 | 56.0 | 7.7 | 13.8% | 1.35 |
| 99th percentile | 59.6 | 8.5 | 14.2% | 1.67 | 53.3 | 3.6 | 6.8% | 1.47 | 85.0 | 14.3 | 16.8% | 2.06 |
| 99.5th percentile | 73.3 | 10.7 | 14.6% | 2.06 | 66.6 | 8.4 | 12.6% | 1.84 | 117.4 | 23.6 | 20.1% | 2.84 |
Changes of AST/ALT ratios according to different percentiles in 14 subgroup cohorts
As the AST/ALT ratio is clinically used for differential diagnosis of liver diseases, we investigated URL values of the AST/ALT ratio (Supplementary Table SI). In men, the URL using the 97.5th value was 2.20, whereas for women it was 2.37. However, when the URL using the 95th value was calculated, 1.95 and 2.09 were suggested for men and women, respectively.
Chronological changes in four liver enzyme parameters in the 14 subgroup cohorts.
We compared the time-dependent changes in four liver enzyme associated parameters using the URL of 97.5th percentile values by absolute mean value differences among the 14 subgroups by age group and gender (Figure 1 B). ALT in men only showed consistent decremental changes according to age, not only in a chronological manner, but also in cross-sectional views at 3 timepoints. GGT in women also presented plausible incremental changes according to age at chronological and cross-sectional timepoints, with less statistical significance compared to ALT in men. Other than these combinations, no obvious changes in other variables in both genders showed significant time-dependent trends, as expected.
As we expanded our analysis to URLs using 95th, 99th and 99.5th values, the observed shapes of time-dependent changes in four parameters in 14 subgroups were diverse, including incremental, decremental, V-shaped, and A-shaped (Supplementary Table SII). Interestingly, decremental changes in ALT of men and incremental changes in GGT of women became more prominent, as observed in Figure 1 B with 97.5th URLs.
Discussion. In this study, we have presented new URL values in a large nationwide representative cohort in South Korea. Interestingly, URLs using four different percentile values (95th, 97.5th, 99th and 99.5th) suggested higher cut-offs than current standards. We suggest that different URLs from our results could be adapted for various purposes, including screening large populations in hepatitis-endemic regions.
In our study, interesting phenomena were noted among associations between age and changes in liver enzymes over time, when we further analyzed the variables by gender and age groups. First, the inverse relationship of ALT and age might be predominant in men rather than women. Interestingly, similar patterns were observed in a previous study of the Korean population [8, 9]. Even though age is an important independent clinical factor for various diseases, our results show that geriatric change in men would not be associated with liver dysfunction in an apparently healthy population. Based on previous studies highlighting the possibly complex relationship between metabolic syndrome or insulin resistance and unhealthy normal ALT levels [10, 11], we hypothesize that in men, liver protective mechanisms might be activated more efficiently than in women as aging proceeds, and therefore show a considerable decrease in ALT chronologically.
Second, taking into account the effects of the AST/ALT ratio when establishing the reference interval might also be recommended in both genders, which appears to be in line with the previous findings [12]. Since it is not practical to develop age-specific URLs in the adult population for a single laboratory, the purpose of this study was to suggest the least vulnerable parameter from a chronolocial viewpoint. The relative stability of AST/ALT ratios across 14 retrospective subgroup cohorts in our study might imply underestimated clinical utility of this ratio for the healthy population.
The fundamental limitation of our study is the selection bias associated with any population-based retrospective cohort. However, this is a large, nationwide population study, which promotes the statistical reliability of the results. Another limitation is associated with definition of the reference population, because we did not include the current standard diagnostic procedure of a liver biopsy in this study.
In conclusion, we investigated age- and gender-specific URLs in individuals without liver diseases using a large nationwide database. Although it is reassuring that the clinical utility of overparticular age-specific URLs in liver enzymes appears to be minimal, dynamic chronological trends in liver enzymes according to different age and gender groups from our study should be considered in the process of reference interval establishment.