Introduction
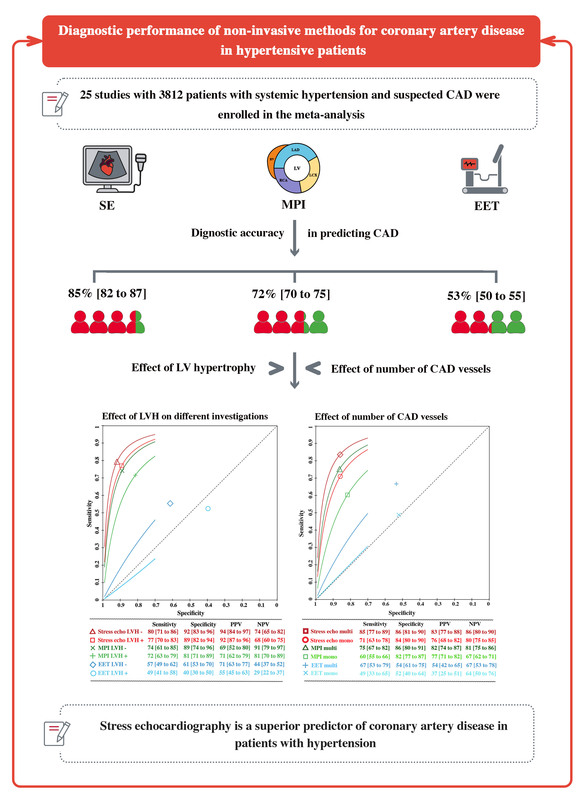
Coronary artery disease (CAD) is the leading cause of morbidity and mortality worldwide [1]. Arterial hypertension (AH) is a well-established risk factor for the development and progression of atherosclerosis and CAD [2]. The pathophysiology of hypertension involves chronic mechanical stress on the arterial wall, leading to increased shear stress, turbulence, and oscillatory shear index. Together with the other conventional risk factors, these processes contribute to the formation of atherosclerotic lesions and subsequent development of CAD [1, 3]. Assessing the prognosis of hypertensive patients is crucial in clinical practice because it is closely associated with a two-fold increase in the risk of developing CAD. Hence, prevention, detection, and management of AH are essential in reducing its burden on society and in improving patient outcome [4]. Non-invasive diagnostic investigations of CAD play a crucial role in the evaluation and optimization of clinical management of these patients [5, 6]. However, the exercise electrocardiography test (EET) faces a significant challenge due to its high rate of false-positive responses. This is primarily due to reduced coronary flow reserve, even when obstructive CAD is not present [7, 8]. On the other hand, functional tests in the form of stress echocardiography (SE) and myocardial perfusion imaging (MPI) provide superior diagnostic accuracy with higher sensitivity and specificity for detecting significant CAD [9–11]. Although new diagnostic techniques and advanced therapeutic approaches have been developed, the non-invasive diagnosis of CAD in hypertensive patients often raises uncertainties, mostly due to left ventricular hypertrophy (LVH) [12]. This does not preclude the important role of the recently developed high accuracy coronary computed tomography angiography (CCTA) [13, 14]. The aim of this meta-analysis was to evaluate the diagnostic accuracy of different non-invasive functional investigations in detecting significant (> 50%) CAD in hypertensive patients.
Material and methods
Search strategy and selection criteria
We adhered to the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15]. As our study was a meta-analysis, obtaining Institutional Review Board (IRB) approval or patient informed consent was unnecessary.
To shape the clinical question and develop the search strategy, we utilized a PECOS model which included parameters for population, intervention, comparison, outcomes, and study design (Supplementary Table SI).
The following databases were searched until February 27th, 2024: PubMed-Medline, EMBASE, Scopus, Google Scholar, the Cochrane Central Registry of Controlled Trials, and ClinicalTrial.gov. The following keywords were used: “Coronary artery disease” OR “CAD” OR “Ischemic heart disease” OR “IHD” AND “Arterial hypertension” AND “Non-invasive diagnostic” OR “Stress echocardiography” OR “Stress echo” OR “Dipyridamole echocardiography” OR “Dobutamine stress echocardiography” OR “ Exercise electrocardiography test” OR “EET” OR “Myocardial perfusion imaging” OR “MPI” AND “Accuracy” (Supplementary Table SII).
Additional searches for potential studies were conducted by reviewing the references of review articles and abstracts from relevant congresses such as the scientific sessions of the European Society of Cardiology (ESC), the European Atherosclerosis Society (EAS), the American Heart Association (AHA), the American College of Cardiology (ACC), and the European Association of Cardiovascular Imaging (EACVI). The wild-card term “*” was used to increase the search sensitivity. The search was limited to human studies published in English, without any applied filters. Each article was evaluated independently by two reviewers (S.B. and I.B.). When there was uncertainty about the suitability of a paper the senior investigator (M.Y.H.) was consulted. The remaining articles were assessed in full text by the same two researchers who extracted and analyzed the data. Usually, data were compared with the original articles and then errors were corrected. The Newcastle-Ottawa Scale (NOS) tool was used to assess the risk of bias in each study. This tool assesses three domains: selection, compatibility and exposure of reported results. The investigators judged the risk of bias in each study as “low”, “high”, or “unclear” [16, 17]. Articles were considered eligible if they reported the diagnostic accuracy in patients with AH: a) studies investigating diagnostic accuracy of non-invasive methods in AH patients; b) studies reporting diagnostic accuracy of significant CAD and/or in comparison of left ventricle hypertrophy or number of diseased vessels; and c) enrolled population of adults aged ≥ 18 years. Exclusion criteria were: i) insufficient statistical data to test the diagnostic accuracy, ii) patients without AH, iii) studies not in humans, and iv) ongoing studies (unless they had reported relevant interim results).
Outcome variables
The main clinical endpoint was the diagnostic accuracy of the non-invasive functional investigations including exercise electrocardiography test (EET), stress echocardiography (SE) and myocardial perfusion imaging (MPI). The secondary endpoint was the effect of left ventricular hypertrophy (LVH), number of diseased vessels and the different CAD territories on diagnostic accuracy. In addition, we evaluated the diagnostic accuracy of SE in patients using two stress modalities: pharmacologic and exercise SE. Moreover, we assessed the accuracy of dobutamine (Dob) compared with dipyridamole (Dip) stress echocardiography.
Significant CAD was defined as ≥ 50% coronary luminal stenosis of at least one major epicardial vessel on conventional coronary angiography. Multivessel disease (MVD) was defined as luminal stenosis in at least two major coronary arteries or in one coronary artery in addition to ≥ 50% stenosis of the left main stem.
Data synthesis and statistical analysis
The meta-analysis was conducted using RevMan software (Review Manager [RevMan] Version 5.1, The Cochrane Collaboration, Copenhagen, Denmark), with two-tailed p < 0.05 considered significant. The baseline characteristics are reported as median and range. Mean and standard deviation (SD) values were estimated using the method described by Hozo et al. [18]. Forest plots were used as the standard method to present the results of individual studies and meta-analyses. We used hierarchical summary receiver operating characteristic (ROC) analysis with the Rutter and Gatsonis model to assess the baseline diagnostic accuracy of the non-invasive investigations [19]. The diagnostic random-effects model was used to compute summary sensitivity and specificity, along with 95% confidence intervals, based on true positive (TP), true negative (TN), false positive (FP), and false negative (FN) values. The summary point obtained from the hierarchical ROC analysis was then used to calculate the positive likelihood ratio (LR+), negative likelihood ratio (LR-), positive predictive value (PPV), negative predictive value (NPV), and diagnostic odds ratio (DOR). For studies that did not provide optimal cut-off values, we created the ROC curve and identified the optimal cut-off as the point on the ROC curve closest to 0.1 in x-y coordinates [19]. The potential interaction between demographic and clinical indices with accuracy of non-invasive investigations was further explored by meta-regression. Meta-regression coefficients and corresponding p-values are reported. We used the random-effects model for the meta-analyses, and heterogeneity between studies was evaluated using the Cochrane Q test and I2 index. I2 < 25% indicated low, 25–50% moderate, and > 50% high heterogeneity. To assess the additive (between-study) component of variance, the reduced maximum likelihood method (tau2) incorporated the occurrence of residual heterogeneity into the analysis [20]. Publication bias was assessed using visual inspections of funnel plots and Egger’s test.
Results
Characteristics of included studies
The initial search identified 2468 articles, which were screened for relevance, resulting in 1278 articles. After a stringent selection process, the meta-analysis included 25 studies comprising 3812 hypertensive patients with known or suspected CAD [21–45] (Supplementary Figure S1). Diagnostic accuracy in 10 studies was evaluated only by one method [21, 23, 25, 30, 32, 35, 40, 42, 44, 45] and the remaining 15 papers reported two or more diagnostic methods [22, 24, 26, 27, 28, 29, 31, 33, 34, 36, 37, 38, 39, 41, 43]. Fourteen studies reported LVH [21, 23, 24, 26, 28, 29, 20, 31, 33, 34, 41, 42, 43, 45] and 9 reported the number of diseased vessels and/or the different territories of CAD [26, 27, 29, 30, 34, 35, 36, 42, 43]. The characteristics of the included studies are shown in Table I.
Table I
Main characteristics of studies included in the meta-analysis
| Study (trial) year | Study design | Location | Population | Sample size | Non-invasive modalities | LV hypertrophy | Prediction [months] |
|---|---|---|---|---|---|---|---|
| Wroblewski 1982 | Retrospective observational study | USA | AH with CAD suspected | 37 | EET | R | Significant SCAD |
| Picano 1988 [22] | Prospective observational study | Italy | AH with CAD suspected | 63 | EET Exercise echocardiography | NR | Significant CAD |
| Prisant 1992 [23] | Prospective observational study | USA | AH with CAD suspected | 92 | MPI | R | Significant CAD |
| Massie 1993 [24] | Prospective observational study | USA | AH with CAD suspected | 226 | EET MPI | R | Significant CAD |
| Tsuda 1993 [25] | Prospective observational study | Japan | AH with CAD suspected | 51 | EET | NR | Significant CAD |
| Senior 1996 [26] | Prospective observational study | UK | AH with CAD suspected | 43 | EET Dob echocardiography | R | Significant CAD MVD |
| Schillaci 1997 [27] | Prospective observational study | Italy | AH with CAD suspected | 40 | EET Dip echocardiography MPI | NR | Significant CAD MVD |
| Astarita 1998 [28] | Prospective observational study | Italy | AH with CAD suspected | 42 | Dip echocardiography MPI | R | Significant CAD |
| Elhendy 1998 [29] | Prospective observational study | Egypt Netherlands | AH with CAD suspected | 84 | Dob echocardiography MPI | R | Significant CAD MVD |
| Ho 1998 [30] | Prospective observational study | Taiwan | AH with known CAD suspected | 101 | Dob echocardiography | R | Significant CAD MVD |
| Fragasso 1999 [31] | Prospective observational study | Italy | AH with CAD suspected | 101 | Dob echocardiography Dip echocardiography MPI | R | Significant CAD |
| Arrif 2000 [32] | Prospective observational study | UK | AH with CAD suspected | 30 | Dob echocardiography | NR | Significant CAD |
| Maltagliati 2000 [33] | Prospective observational study | Italy | AH with CAD suspected | 59 | EET Exercise echocardiography | R | Significant CAD |
| Pasierski 2001 [34] | Prospective observational study | Poland | AH with CAD suspected | 197 | EET Dob echocardiography Exercise echocardiography | R | Significant CAD MVD |
| Elhendy 2001 [35] | Prospective observational study | USA | AH with CAD suspected | 137 | MPI | NR | Significant CAD MVD |
| Astarita 2001 [36] | Prospective observational study | Italy | AH with CAD suspected | 53 | Dip echocardiography MPI | NR | Significant CAD MVD |
| Cortigiani 2003 [37] | Prospective observational study | Italy | AH with CAD suspected | 35 | EET Dip echocardiography | NR | Significant CAD |
| Milosavljevic 2005 [38] | Prospective observational study | Serbia | AH with CAD known or suspected | 127 | Dip echocardiography Dob echocardiography | NR | Significant CAD |
| Nishida 2005 [39] | Retrospective observational study | Japan | AH with CAD suspected | 83 | EET MPI | NR | Significant CAD |
| Michaelides 2007 [40] | Prospective observational study | Greece | AH with CAD suspected | 179 | MPI | NR | Significant CAD |
| Aggeli 2007 [41] | Prospective observational study | Greece | AH with CAD suspected | 50 | Stress echocardiography MPI | R | Significant CAD |
| Michaelides 2009 [42] | Prospective observational study | Greece | AH with CAD suspected | 382 | EET | R | Significant CAD MVD |
| Lu 2010 [43] | Prospective observational study | Italy | AH with CAD suspected | 76 | EET Dob echocardiography Exercise echocardiography MPI | R | Significant CAD MVD |
| Cortigiani 2011 [44] | Retrospective observational study | Italy | AH with CAD suspected | 1411 | Dob echocardiography | NR | Significant CAD |
| Zimarino 2016 [45] | Retrospective observational study | Italy | AH with CAD suspected | 113 | EET | R | Significant CAD |
The mean age of patients was 52.2 ±7.8 years and 44.5% were female. 51.8% of the patients had CAD, 42.3% were smokers, 19.7% diabetic and 37.2% had dyslipidemia (Supplementary Table SIII).
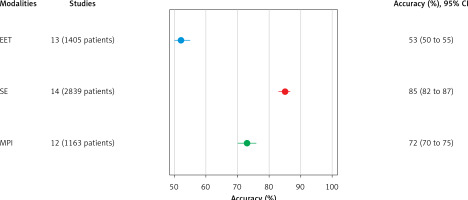
Diagnostic accuracy of non-invasive methods in detecting significant CAD
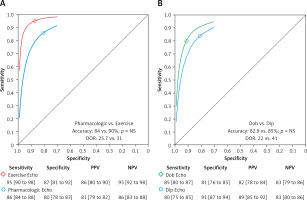
SE with a summary sensitivity of 87%, summary specificity 81%, and 85% accuracy was the most powerful predictor of significant CAD followed by MPI with summary sensitivity of 81%, summary specificity of 64% and accuracy of 72%. EET was the investigation with the lowest accuracy with summary sensitivity of 53%, summary specificity of 51% and accuracy of 53% (Figures 1, 2). Positive and negative predictive values were, respectively, 82% and 87% for SE, 71% and 76% for MPI and 56% and 48% for EET (Table II). The predictive value of significant CAD for SE measured by different modalities (pharmacologic vs. physical exercise) was also assessed. The results showed no difference between the accuracy of the two techniques (84% vs. 90%; p = NS; Figure 3 A, Supplementary Figure S2). Although dobutamine SE had modestly higher summary sensitivity (85% vs. 80%) and lower summary specificity (81% vs. 91%) compared to dipyridamole SE, the accuracy was not different between the two SE modalities (83% vs. 85% Figure 3 B, Supplementary Figure S2).
Table II
Diagnostic accuracy of non-invasive methods in detecting significant CAD
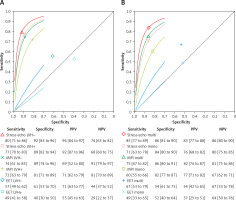
Effect of left ventricular hypertrophy on diagnostic accuracy of non-invasive methods
Left ventricular hypertrophy did not have a significant impact on the diagnostic accuracy of the two stress techniques, SE and MPI. In both investigations the accuracy of the diagnostic indices was similar in patients with and without hypertrophy. The accuracy was not different in SE (85% vs. 81%, p > 0.05) or MPI (75% vs. 71%, p > 0.05). However, EET accuracy was lower in patients with LVH compared to those without (41% vs. 58%, p = 0.03; Figure 4 A, Supplementary Figure S3).
Effect of number of diseased vessels on diagnostic accuracy of investigations
Regardless of the non-invasive diagnostic investigation used, patients with MVD had higher sensitivity, specificity, positive predictive value, negative predictive value, and accuracy compared to those with single-vessel disease. The summary sensitivity of SE was 85%, summary specificity 86% and accuracy 86% in detecting MVD while in single vessel disease respective values were 71%, 84% and 78%. Likewise, the accuracy of MPI and EET in detecting MVD compared to single vessel disease was significantly higher (81% vs. 71% and 60% vs. 50%; p < 0.05 for both) (Figure 4 B, Supplementary Figure S4).
The regional accuracy of SE and MPI was similar for LAD and LCx artery stenosis, but there was a trend towards lower sensitivity for RCA stenosis. This may be due to the RCA’s anatomical position, which makes it more challenging to visualize and assess accurately, potentially leading to reduced sensitivity and specificity. Additionally, collateral circulation can obscure stenosis detection, complicating accurate diagnosis with these imaging techniques (Supplementary Figure S5).
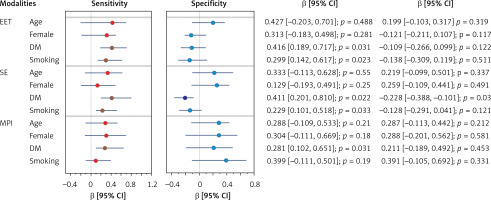
Interaction of demographic and clinical indices with accuracy of non-invasive methods
Demographic and clinical indices were tested for possible interaction with accuracy of the non-invasive investigations. Positive interactions were found for diabetes mellitus (β = 0.411; p = 0.02) and smoking (β = 0.229; p = 0.03) with sensitivity of SE and EET (β = 0.416 and β = 0.299; p < 0.05, respectively) and diabetes with sensitivity of MPI (β = 0281; p = 0.03). A negative interaction was found only between diabetes (β = –0.228; p = 0.03) and the specificity of SE. Other factors did not have any interaction with the specificity of other modalities (Figure 5, Supplementary Figures S6–S8).
Risk of bias assessment
The assessment of the risk of bias in the included studies using NOS showed that most studies had a moderate to high quality level in defining objectives and primary outcomes (Supplementary Table SIV). Also, there was no evidence of publication bias, evaluated by Egger’s test, for our findings.
Discussion
Findings
The findings of this meta-analysis, which included 25 studies and a total of 3,812 hypertensive patients with either known or suspected coronary artery disease, are as follows: a) Stress echocardiography is a superior predictor of significant (> 50%) CAD in patients with hypertension compared to the two other non-invasive functional investigations, EET and MPI. b) The accuracy of the two SE modalities was similar, even when dobutamine or dipyridamole was used. c) The accuracy of the three non-invasive diagnostic investigations was higher in patients with multivessel coronary disease compared to those with single-vessel disease. d) The diagnostic accuracy of SE and MPI was not impacted by left ventricular hypertrophy; however, that of EET was lower in patients with hypertrophy compared to those without.
Data interpretation
Despite advances in early diagnosis and treatment of AH, related morbidity and mortality rates continue to be of significant concern. Evaluating the prognosis of hypertensive patients is a critical aspect of clinical practice due to the strong relationship between hypertension and the risk of developing CAD [2, 3], even when subclinical. Accurate assessment of the diagnostic value of non-invasive investigations for detecting CAD is essential for effective management of patients with hypertension [4, 5]. Our meta-analysis shows that SE has significantly higher accuracy than myocardial perfusion imaging and exercise stress testing, and thus should provide incremental diagnostic value for the detection and localization of significant CAD.
EET is considered a potentially useful diagnostic tool for CAD screening due to its simplicity, low cost, and safety [46] with significant prognostic power. However, many studies have demonstrated its relatively poor accuracy for detecting CAD, even in symptomatic individuals due to the co-existence of bundle branch blocks, premature test termination, etc. A considerable number of hypertensive patients experience chest pain/discomfort, particularly with exercise. In these patients, EET specificity for diagnosing significant CAD has been proved limited, particularly in those with left ventricular hypertrophy and/or pre-existing ECG abnormalities [47]. In patients without significant ECG abnormalities at rest, frequently seen in hypertension clinics, diagnostic accuracy of EET is even lower [48, 49]. Such poor accuracy has led the recommendations to discourage the use of exercise testing as a screening tool [7, 47,48]. These findings are supported by our results, which showed that EET has low accuracy in all hypertensive individuals.
Our results have shown respectable accuracy of MPI for detecting CAD, irrespective of the presence of LVH [7, 50] but still inferior to SE. Despite that, the risk of MPI associated radiation exposure, particularly in the young and in women, limits the potential for using MPI as a screening functional investigation in the general population [51]. EET and MPI assess electric and myocardial perfusion signs of ischemia, respectively, particularly transmural. Recently, the development of CCTA has added extra power to the non-invasive armamentarium of diagnosing significant CAD, with its ability to provide a detailed anatomical description of the location and severity of branch stenosis. Whenever in doubt about the stenosis grade, recent guidelines offer class 1 recommendation for functional tests for detecting myocardial ischemia, even without CCTA, in intermediate- to high-risk patients [52]. Indeed, a large study including 1000 patients with possible stable CAD demonstrated higher efficiency of functional tests including SE, positron emotion tomography (PET), non-invasive fractional flow reserve (FFRCT) and cardiac magnetic resonance imaging [8] in diagnosing significant CAD. Although these results are important, their wide implementation could be limited because of the known CT-related limitations, including radiation, subjectivity, cost-effectiveness ratio, cost-utility ratio and availability, particularly in developing countries [7, 8,21]. On the other hand, in our analysis SE was found to be the strongest predictor of significant CAD through accurate evaluation of ischemic myocardial wall motion abnormalities. Such high accuracy is irrespective of the pharmacological modality used, dobutamine or dipyridamole. Based on this finding the recommendation of generalized use of SE as a screening test in hypertensive patients can be justified, particularly because of its additional benefits: having zero radiation, being patient friendly and avoiding possible claustrophobia of other scanning tubes. The cost-effectiveness ratio and cost-utility ratio, and the need for a certain degree of specialized knowledge, are additional benefits for SE, particularly in these patients. Despite such benefits, it must be mentioned that some of those patients presenting with exertional symptoms might not prove to have significant coronary stenosis as a cause of their symptoms but either vasospastic disease or microcirculation disease or both. While SE might show wall motion abnormalities in the former [53] it might not demonstrate significant evidence for ischemia in the latter [54], based on the limited available evidence in the literature. These findings advocate for broader clinical implementation of SE because of its cost-effectiveness, patient-friendliness, and lack of radiation exposure. This study also provides strong evidence for revising current diagnostic protocols, emphasizing the need for wider use of SE for early diagnosis of coronary artery disease and hence improvement of patient clinical outcomes.
Clinical implication
The findings of our meta-analysis have significant clinical implications. Hypertension is one of the commonest presentations in cardiology clinics and general practice, irrespective of symptoms. While age and other comorbidities may impact development of co-existing symptoms, such patients, particularly those with long standing hypertension and family history of CAD or stroke, warrant further investigations in order to optimize their clinical management and prevent them developing serious acute events. Our results support the generalized use of SE in such individuals, particularly those who cannot tolerate physical exercise and when MPI, with its special requirements, is not available. The use of more sophisticated echocardiographic modalities including speckle tracking echocardiography for the assessment of myocardial deformation is expected to increase the accuracy of SE in diagnosing significant CAD in these patients.
Limitations
Our meta-analysis has obvious limitations. The data obtained do not allow conclusions to be drawn in relation to the severity of CAD stenosis. We could not include in our analysis data on CMR and PET techniques, because of the limited number of available publications, which would undermine the relevance of the statistical analysis. Due to the limited number of published articles on the use of speckle tracking echocardiography for the assessment of myocardial deformation in these patients, this analysis could not be performed. Also, due to the limited number of available studies on the investigation of hypertensive patients based on the antihypertensive therapy and duration of hypertension, these data were not included in the analysis. Moderate heterogeneity across some studies was evident in various risk of bias and analyses; therefore the random-effects method was applied to lessen the impact of this heterogeneity.
Conclusions
This meta-analysis revealed the powerful diagnostic value of stress echocardiography, irrespective of the used modality, in detecting significant coronary artery disease in patients with systemic hypertension. Future analysis of other functional tests and advanced echocardiographic modalities could provide more specific indications for the optimum patient stratification.