The pelvis is composed of multiple bones that connect the spine to the bones of the lower limbs [1]. Pelvic fractures are often caused by high-energy trauma, such as car accidents and falls from heights. There are abundant blood vessels near the pelvis, and acute haemorrhage is one of the most common and serious complications of high-energy pelvic fractures [2]. Haemodynamic instability is a clinical feature of haemorrhagic pelvic fractures and can increase the risk of death to 30–60% [3, 4].
It is still unclear what the best treatment choice for early-stage haemorrhagic pelvic fracture care is. Immediate external fixation is an effective method for controlling venous bleeding. For arterial haemorrhage, vascular angiography and embolisation are the main methods used; early identification and embolisation of arterial haemorrhage can improve mortality [5]. However, delayed arterial bleeding, which is more difficult to detect and also more dangerous, is less commonly reported. We report the first case of multiple arterial haemorrhage 3 days after admission in a haemodynamically stable patient with a pelvic fracture and analyse the causes and clinical course. We hope this report provides valuable clinical information on the prevention and identification of delayed arterial haemorrhage in pelvic fracture patients.
A 55-year-old female patient was admitted to our hospital on 9 August 2023, with fractures of the superior and inferior ramus of the left pubis. The patient had both diabetes and hyperlipidaemia, which were treated with medication. Examination after admission showed a blood pressure of 124/79 mm Hg, heart rate of 94 bpm and body temperature of 37.2℃. Her numerical rating scale (NRS) pain score was 3, Morse Fall Scale score was 35, and her Caprini score was 7. Computed tomography (CT) revealed multiple fractures of the left ilium and the superior and inferior ramus of the pubis (Figure 1 A): multiple slightly high-density nodules on the medial side of the left pelvic wall were considered a haematoma. Laboratory test results showed a red blood cell count of 3.59 × 1012/l, haemoglobin at 106 g/l, triglycerides at 2.26 mmol/l, lipoprotein at 0.73 g/l, apolipoprotein E at 27.9 mg/l, and glucose at 17.4 mmol/l.
Figure 1
A – 3D reconstruction showed left pubic upper and lower limb fractures. B – CT showed fluid and blood accumulation in the abdominal and pelvic cavities and in the retroperitoneum
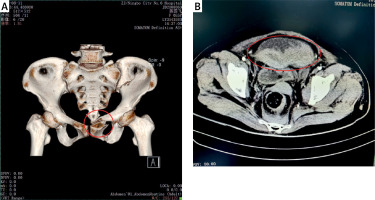
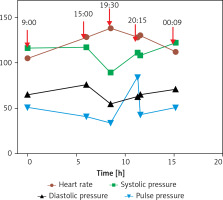
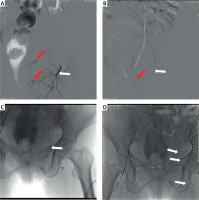
At 9:00 on 11 August, the patient complained of unbearable abdominal distension and pain. Her blood pressure was 116/65 mm Hg and heart rate, 105 bpm. Since the patient had not defecated for 3 days after admission, constipation was considered the cause. The nurse followed the doctor’s advice and administered a 20-mL glycerol enema. The patient’s abdominal pain was relieved after defecation. However, at 15:00, the nurse found that the patient still had abdominal pain, with a swollen abdomen and obvious tenderness in the lower abdomen. The patient’s blood pressure was 117/76 mm Hg, and heart rate was 128 bpm. Arterial haemorrhage was suspected, and laboratory examination showed a red blood cell count of 2.32 × 1012/l and haemoglobin at 69 g/l. CT showed fluid and blood accumulation in the abdominal and pelvic cavities and the retroperitoneum; mixed-density shadows were seen in the right lower abdominal cavity (Figure 1 B). An hour later, an enhanced CT scan suggested active bleeding. At 17:45, left internal iliac artery angiography and embolisation were performed. Arteriography showed damage to the left obturator artery, left superficial epigastric artery, and left superficial perineal artery. At 19:30, the patient’s blood pressure had decreased to 89/55 mm Hg, and her heart rate was 138 bpm. Three bleeding sites were treated with spring plug embolisation (Figures 2 B–D). Treatment ended at 20:15, and the patient was infused with three units of O-type red blood cells at 20:32; the patient’s blood pressure was 108/65 mm Hg, and her heart rate was 130 bpm. At 00:09 on 12 August, the patient was infused with 310 ml of O-type Rh-positive frozen plasma, and her heart rate dropped to 112 bpm with a blood pressure of 122/71 mm Hg. On 13 August, she had a red blood cell count of 3.05 × 1012/l and haemoglobin at 91 g/l (Figure 3).
Figure 2
A – Angiography of the left superficial epigastric artery. B – Angiography of the left superficial perineal artery. C – Angiography of the left obturator artery. D – Spring-plug embolisation was performed at the three identified bleeding sites. The red arrows indicate significant bleeding, and the white arrows indicate the embolisation site
On 17 August, the patient had pelvic fracture fixation surgery and was discharged on 24 August with a blood pressure of 100/58 mm Hg and heart rate of 89 bpm.
The commonly damaged arteries in pelvic fractures include the iliac lumbar, superior gluteal, inferior gluteal, obturator, and internal pudendal arteries [6]. Pelvic fractures caused by blunt trauma are prone to damaging the superior gluteal artery [7], and the location of the sciatic notch is a risk factor for superior gluteal artery injury [8]. Fractures of the lateral part of the sacrum can damage the posterior branch of the internal iliac artery, including the iliac lumbar and superior gluteal arteries.
In this case, the fracture of the superior and inferior branches of the pubis meant a risk of damage to the obturator and the internal pudendal arteries [9]. Delayed bleeding from pelvic fractures is rare; the reason for delayed onset is believed to be the slow formation and rupture of a traumatic pseudoaneurysm caused by vascular injury during the initial trauma period. However, the CT at admission in this case did not indicate a potential risk of bleeding in these three blood vessels. The patient’s haemodynamics remained stable until the onset of abdominal pain 72 h later. Damage to the superficial abdominal artery in pelvic fractures has not been reported previously. The superficial abdominal artery originates from the femoral artery and is distributed in the superficial fascia and skin below the anterior abdominal wall. Compared to other arterial vessels mentioned above, it is relatively far from the pelvis.
Abdominal pain is the main symptom of various diseases, including intestinal diseases and arterial bleeding [10]. In this case, when the patient was constipated and her blood pressure and heart rate did not change significantly, the nurse first considered the abdominal pain to be caused by constipation. The patient’s abdominal pain did alleviate after defecation. However, she experienced a significant increase in heart rate after defecation. Because of this, we suspect that the arterial bleeding was caused by defecation; the patient needed to change her position to defecate as she was unable to get out of bed and walk. Although pelvic external fixation can limit and reduce secondary vascular injury in patients [11], it does not completely avoid the potential risks of muscle activity during defecation or changes in posture.
Timely identification of arterial bleeding was crucial for rescuing this patient. Delaying angiography for over 60–90 min or embolisation for more than 3 h can significantly increase mortality [12, 13]. In the present study, the heart rate of the patient continued to rise with the occurrence of arterial bleeding (Figures 2 A). This suggests that a temporary stabilization of blood pressure is achieved by a compensatory increase in heart rate. This led to a continuous reduction in the pulse pressure difference between systolic and diastolic blood pressure, although the change in blood pressure itself was minimal. After 4 h, the patient’s blood pressure significantly decreased, and there was a risk of shock. Focusing on the heart rate and blood pressure changes helps rapidly identify arterial bleeding.
The limitation of this report is that there is no substantial evidence to confirm the cause of delayed bleeding or damage to the superficial abdominal artery. Due to the lack of cases, further analysis of the mechanism of delayed arterial bleeding is not currently possible, though as reports increase, we will continue to conduct further research.
In conclusion, haemodynamically stable patients with pelvic fractures may still have delayed multiple arterial bleeding. The cause of the resulting arterial haemorrhage may be related to changes in patient mobility or posture. When patients have abdominal pain symptoms, nurses should pay attention to haemodynamic changes such as heart rate to identify potential active bleeding. Nursing staff rounds are essential for the timely intervention of arterial bleeding.