Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
Cutaneous ulcers in anti-MDA5-positive dermatomyositis with rapidly progressive interstitial lung disease: a multicentre retrospective cohort study
1
Department of Rheumatology and Immunology, The Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu, China
2
Department of Rheumatology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
3
Department of Rheumatology and Immunology, Wuxi People’s Hospital, Wuxi, Jiangsu, China
4
Department of Rheumatology and Immunology, Huai’an First People’s Hospital, Huai’an, Jiangsu, China
5
Department of Rheumatology and Immunology, The First People’s Hospital of Changzhou, Changzhou, Jiangsu, China
6
Department of Rheumatology and Immunology, Affiliated Hospital of Nantong University, Nantong, Jiangsu, China
7
Department of Rheumatology and Immunology, Northern Jiangsu People’s Hospital, Yangzhou, Jiangsu, China
8
Department of Rheumatology and Immunology, Changzhou No. 2 People’s Hospital, Changzhou, Jiangsu, China
9
Department of Rheumatology and Immunology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, Jiangsu, China
10
Department of Rheumatology and Immunology, The First Affiliated Hospital of Soochow University, Suzhou, Jiangsu, Chin
11
Department of Rheumatology and Immunology, Jiangsu Province Hospital of Chinese Medicine, Nanjing, Jiangsu, China
12
Department of Rheumatology and Immunology, Nanjing First Hospital, Nanjing, Jiangsu, China
13
Department of Rheumatology and Immunology, Xuzhou Central Hospital, Xuzhou, Jiangsu, China
14
Department of Rheumatology and Immunology, Yancheng No. 1 People’s Hospital, Yancheng, Jiangsu, China
15
Department of Rheumatology and Immunology, Zhongda Hospital Southeast University, Nanjing, Jiangsu, China
16
Department of Rheumatology and Immunology, The First People’s Hospital of Lianyungang, Lianyungang, Jiangsu, China
17
Department of Rheumatology and Immunology, Wuxi No. 2 People’s Hospital, Wuxi, Jiangsu, China
18
Department of Rheumatology and Immunology, The Affiliated Suqian First People’s Hospital of Nanjing Medical University, Suqian, Jiangsu, China
Submission date: 2023-09-04
Final revision date: 2024-01-17
Acceptance date: 2024-01-20
Online publication date: 2024-12-16
Corresponding author
Zhichun Liu
Department of Rheumatology and Immunology, Second Affiliated Hospital of Soochow University, Suzhou, 215004, China, China
Department of Rheumatology and Immunology, Second Affiliated Hospital of Soochow University, Suzhou, 215004, China, China
KEYWORDS
dermatomyositisanti-MDA5+ dermatomyositisrapidly progressive interstitial lung diseaseproximal muscle involvementheliotrope rashrisk factors
TOPICS
ABSTRACT
Introduction:
To identify the clinical characteristics and risk factors for cutaneous ulcers in patients with anti-melanoma differentiation-associated gene 5 antibody-positive dermatomyositis (anti-MDA5+ DM) combined with rapidly progressive interstitial lung disease (RPILD).
Material and methods:
We conducted a retrospective cohort study on the medical records of patients enrolled from the Nanjing Medical University Myositis-associated ILD cohort (NMMI). The clinical characteristics of patients in the ulcer-positive group were compared with those in the ulcer-negative group by chi-square or Fisher’s exact test. Univariate and multivariate logistic regression analyses were used to assess risk factors for the development of cutaneous ulcers.
Results:
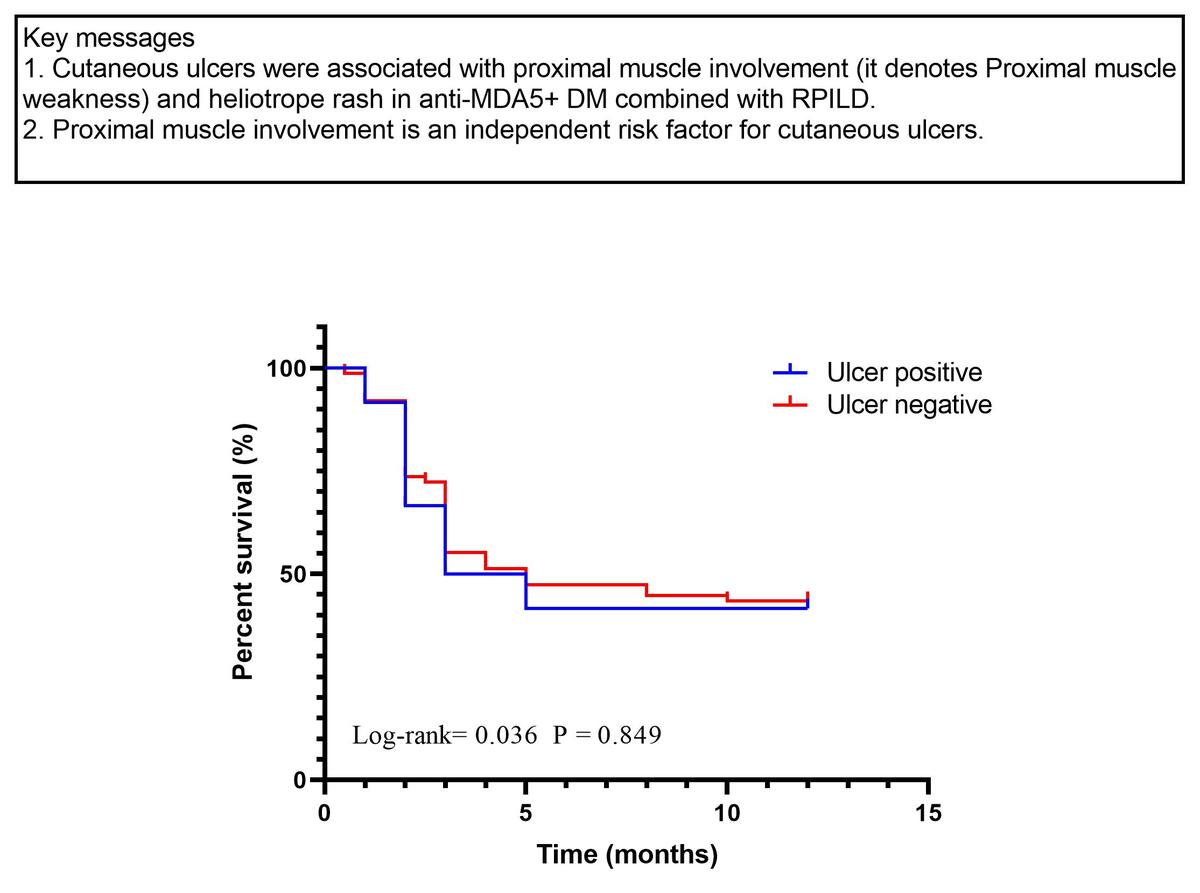
A total of 246 patients with anti-MDA5+ DM were retrospectively enrolled in the study, including 176 females (176/246, 71.54%) and 70 males (70/246, 28.46%), with a female-to-male ratio of 2.51 : 1. Among the 246 patients, a total of 88 cases (88/246, 35.77%) with anti-MDA5+ DM combined with RPILD were further studied, including 55 females (55/88, 62.5%) and 33 males (33/88, 37.5%), with a female-to-male ratio of 1.67 : 1. Twelve patients (12/88, 13.64%) had cutaneous ulcers. In terms of clinical characteristics, patients in the ulcer-positive group had significantly more proximal muscle involvement (83.33% vs. 38.16%, p = 0.003) and more heliotrope rash (83.33% vs. 43.42%, p = 0.010) than in the ulcer-negative group. In univariate analysis, cutaneous ulcers were associated with proximal muscle involvement (OR = 8.103; 95% CI: 1.657–39.625; p = 0.010) and heliotrope rash (OR = 6.515; 95% CI: 1.336–31.773; p = 0.020). In multivariate analysis, cutaneous ulcers were associated with proximal muscle involvement (OR = 6.436; 95% CI: 1.274–32.524; p = 0.024), and proximal muscle involvement was an independent risk factor for cutaneous ulcers.
Conclusions:
We confirmed the association between cutaneous ulcers and proximal muscle involvement and heliotrope rash in patients with anti-MDA5+ DM combined with RPILD. Proximal muscle involvement is an independent risk factor for cutaneous ulcers.
To identify the clinical characteristics and risk factors for cutaneous ulcers in patients with anti-melanoma differentiation-associated gene 5 antibody-positive dermatomyositis (anti-MDA5+ DM) combined with rapidly progressive interstitial lung disease (RPILD).
Material and methods:
We conducted a retrospective cohort study on the medical records of patients enrolled from the Nanjing Medical University Myositis-associated ILD cohort (NMMI). The clinical characteristics of patients in the ulcer-positive group were compared with those in the ulcer-negative group by chi-square or Fisher’s exact test. Univariate and multivariate logistic regression analyses were used to assess risk factors for the development of cutaneous ulcers.
Results:
A total of 246 patients with anti-MDA5+ DM were retrospectively enrolled in the study, including 176 females (176/246, 71.54%) and 70 males (70/246, 28.46%), with a female-to-male ratio of 2.51 : 1. Among the 246 patients, a total of 88 cases (88/246, 35.77%) with anti-MDA5+ DM combined with RPILD were further studied, including 55 females (55/88, 62.5%) and 33 males (33/88, 37.5%), with a female-to-male ratio of 1.67 : 1. Twelve patients (12/88, 13.64%) had cutaneous ulcers. In terms of clinical characteristics, patients in the ulcer-positive group had significantly more proximal muscle involvement (83.33% vs. 38.16%, p = 0.003) and more heliotrope rash (83.33% vs. 43.42%, p = 0.010) than in the ulcer-negative group. In univariate analysis, cutaneous ulcers were associated with proximal muscle involvement (OR = 8.103; 95% CI: 1.657–39.625; p = 0.010) and heliotrope rash (OR = 6.515; 95% CI: 1.336–31.773; p = 0.020). In multivariate analysis, cutaneous ulcers were associated with proximal muscle involvement (OR = 6.436; 95% CI: 1.274–32.524; p = 0.024), and proximal muscle involvement was an independent risk factor for cutaneous ulcers.
Conclusions:
We confirmed the association between cutaneous ulcers and proximal muscle involvement and heliotrope rash in patients with anti-MDA5+ DM combined with RPILD. Proximal muscle involvement is an independent risk factor for cutaneous ulcers.
REFERENCES (24)
1.
DeWane ME, Waldman R, Lu J. Dermatomyositis: clinical features and pathogenesis. J Am Acad Dermatol 2020; 82: 267-81.
2.
Wu W, Guo L, Fu Y, et al. Interstitial lung disease in anti-MDA5 positive dermatomyositis. Clin Rev Allergy Immunol 2021; 60: 293-304.
3.
Quain RD, Werth VP. Management of cutaneous dermatomyositis: current therapeutic options. Am J Clin Dermatol 2006; 7: 341-51.
4.
Narang NS, Casciola-Rosen L, Li S, Chung L, Fiorentino DF. Cutaneous ulceration in dermatomyositis: association with anti-melanoma differentiation-associated gene 5 antibodies and interstitial lung disease. Arthritis Care Res 2015; 67: 667-72.
5.
Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med 1975; 292: 344-7.
6.
Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med 1975; 292: 403-7.
7.
Schaefer-Prokop C, Prokop M, Fleischmann D, Herold C. High-resolution CT of diffuse interstitial lung disease: key findings in common disorders. Eur Radiol 2001; 11: 373-92.
8.
Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 2013; 188: 733-48.
9.
Xu A, Ye Y, Fu Q, et al. Prognostic values of anti-Ro52 antibodies in anti-MDA5-positive clinically amyopathic dermatomyositis associated with interstitial lung disease. Rheumatology (Oxford, England) 2021; 60: 3343-51.
10.
Kurtzman DJB, Vleugels RA. Anti-melanoma differentiation-associated gene 5 (MDA5) dermatomyositis: a concise review with an emphasis on distinctive clinical features. J Am Acad Dermatol 2018; 78: 776-85.
11.
Wolstencroft PW, Fiorentino DF. Dermatomyositis clinical and pathological phenotypes associated with myositis-specific autoantibodies. Curr Rheumatol Rep 2018; 20: 28.
12.
Cao H, Xia Q, Pan M, et al. Gottron papules and gottron sign with ulceration: a distinctive cutaneous feature in a subset of patients with classic dermatomyositis and clinically amyopathic dermatomyositis. J Rheumatol 2016; 43: 1735-42.
13.
Fiorentino D, Chung L, Zwerner J, Rosen A, Casciola-Rosen L. The mucocutaneous and systemic phenotype of dermatomyositis patients with antibodies to MDA5 (CADM-140): a retrospective study. J Am Acad Dermatol 2011; 65: 25-34.
14.
Valenzuela A, Chung L, Casciola-Rosen L, Fiorentino D. Identification of clinical features and autoantibodies associated with calcinosis in dermatomyositis. JAMA Dermatol 2014; 150: 724-9.
15.
Nagashima T, Iwamoto M, Minota S. Gottron sign with ulceration is not a poor prognostic factor in patients with dermatomyositis and interstitial lung disease. J Rheumatol 2017; 44: 1099-100.
17.
Burnouf M, Mahé E, Verpillat P, et al. Cutaneous necrosis is predictive of cancer in adult dermatomyositis. Ann Dermatol Venereol 2003; 130: 313-6.
18.
Mahé E, Descamps V, Burnouf M, Crickx B. A helpful clinical sign predictive of cancer in adult dermatomyositis: cutaneous necrosis. Arch Dermatol 2003; 139: 539.
19.
Nousari HC, Kimyai-Asadi A, Spegman DJ. Paraneoplastic dermatomyositis presenting as erythroderma. J Am Acad Dermatol 1998; 39: 653-4.
20.
Kanbayashi T, Tanaka S, Hatanaka Y, Uchio N, Shimizu J, Sonoo M. Myasthenia gravis with inflammatory myopathy without elevation of creatine kinase. Neuromuscul Disord 2021; 31: 570-3.
21.
Haran M, Schattner A, Kozak N, Mate A, Berrebi A, Shvidel L. Acute steroid myopathy: a highly overlooked entity. QJM 2018; 111: 307-11.
22.
Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: ocular, cardiovascular, muscular, and psychiatric side effects and issues unique to pediatric patients. J Am Acad Dermatol 2017; 76: 201-7.
23.
Zuo Y, Ye L, Chen F, et al. Different multivariable risk factors for rapid progressive interstitial lung disease in anti-MDA5 positive dermatomyositis and anti-synthetase syndrome. Front Immunol 2022; 13: 845988.
24.
Han YY, Jiang T, Zhang ZH, et al. Risk factors of rapidly progressive interstitial lung disease in patients with anti-melanoma differentiation-associated gene 5 antibody-positive dermatomyositis. Sichuan Da Xue Xue Bao Yi Xue Ban 2023; 54: 422-5.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.