Introduction
Fetal growth restriction (FGR) is the failure of the fetus to reach its growth potential [1]. It is commonly assessed by its proxy, small for gestational age (SGA), when full information about growth as a longitudinal measure is not available, as birthweight [2] or fetal weight [3] below the tenth population-based centile [4]. Fetal growth restriction is associated with an increased risk for perinatal morbidity and mortality [5], but in practice most cases of FGR remain undetected prenatally [6].
One approach aimed at improving detection of growth restriction is through the use of customised, rather than population-based growth charts. There is a growing body of evidence supporting the role of customized growth charts in improving detection of FGR and decreasing false positive diagnoses [7–12]. Implementation of customized charts at a population level has also been associated with a decrease in stillbirth [12, 13]. In the UK, the Royal College of Obstetricians and Gynaecologists has recommended the use of a customized fetal weight reference for assessing fetal growth and birthweight [14].
The process for developing customized growth charts is based on three steps: first, developing a statistical model using population data to predict optimal birth weight adjusted for physiological factors – maternal parity, ethnicity, height and weight, and fetal gender; second, identifying and removing from the model pathological factors (such as pre-eclampsia and diabetes) that significantly affect growth in the population; last, the customized optimal birth weight is projected backward for all gestational age points, using an ultrasound-based proportionality curve so that fetal growth measurements at all gestations can be plotted on a customized chart that is based on the individual baby’s growth potential at term [1, 15].
In this study, we aimed to produce a customised birthweight standard based on the significant variables found in a Polish population and compare this to the current in-use neonatal standard in Poland [16].
Material and methods
Data collection
This retrospective cohort study used data from pregnancies at St Sophia’s Hospital, a tertiary maternity centre in Warsaw, Poland with approximately 6800 deliveries per year, and were collected as part of routine patient assessment. The cohort consisted of 5079 cases entered into an electronic maternity record (AMMS – Asseko Medical Management Solutions, Poland) which had complete data on gestation dates, maternal height and weight and pregnancy outcome.
This project had ethical approval from the Centre of Postgraduate Medical Education, Warsaw, Poland.
Study population
All patients admitted to the hospital for maternity care had gestational age routinely verified by first trimester ultrasound (USS) and last menstrual period (LMP). If the difference between LMP and USS was less than 7 days, LMP was used; otherwise USS was used [17]. Maternal height and weight in early pregnancy were recorded during the first appointment. Patient history was recorded in an electronic database. Pathological variables including gestational diabetes, pre-existing diabetes, pregnancy-induced hypertension, pre-existing hypertension, asthma, anaemia and smoking were self-reported as yes/no responses. These were collected via interview, maternity records or from outpatient clinic staff. Pregnancies with ethnicity other than Polish were rare in this medical centre and were not included in this study.
Inclusion/exclusion criteria
Pregnancies with incomplete/invalid data of the critical variables for generating customised centiles (birthweight, gestational age, parity, fetal sex, maternal height and weight) were excluded from this analysis, leaving 4,800 pregnancies. To generate a standard to model optimal birthweight, pregnancies in which there was a pre-term birth (< 37 weeks gestation), multi-fetal pregnancy or congenital anomaly were excluded, leaving 4,270 pregnancies for analysis.
Model performance
The derived physiological coefficients were combined with the standard proportionality curve [15] to provide the gestation related optimal weight (GROW) tool to assess birthweight. To assess suitability for use in Poland, we tested this model’s performance against the in-use Fenton standard [16]. Customised centiles were generated following the above model customising for maternal height, weight, parity and gender. The Fenton centiles were generated using published methods, adjusted only for sex [16]. This was performed on a subset of 4,800 pregnancies that had complete and valid data for calculating centiles. Births were designated as SGA (< 10th centile) according to their respective standards. Subgroups of SGA by each standard were compared for risk of stillbirth, neonatal intensive care unit (NICU) admission or one or more neonatal complications (intraventricular haemorrhage, transient tachypnoea, respiratory distress syndrome, hypoxic ischaemic encephalopathy, broncho-pulmonary dysplasia, sepsis or seizure). Relative risk (RR) with 95% confidence interval and population attributable risk (PAR) were calculated.
Statistical analysis
The method to generate coefficients for customised birth-weight centiles was following that described previously [15]. Multivariate linear regression with stepwise backward elimination was used to obtain coefficients for significant variables with cut-off at probability 0.05. The regression analysis was run on the filtered 4,270 pregnancies.
To allow comparison with previous studies [18–20], the model was centred on a standard mother with height 163 cm, booking weight 64 kg, gestation 280 days and parity zero, and the baby’s sex undefined, i.e. neutral or ‘averaged’ between male and female. As maternal height and weight have a non-linear relationship with birthweight, they were entered as polynomials up to the third power. Pathological factors were included as categorical variables to quantify their effect on birthweight but then excluded when calculating the ‘term optimal weight’ to be free from known pathology. All analyses were performed using Stata (version 15.1; Statacorp, College Station, TX).
Results
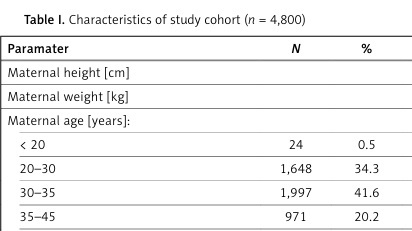
The characteristics of the 4,800 pregnancies with complete data are listed in Table I. Over half (53.4%) of the pregnancies were nulliparous and 8.8% led to preterm birth (< 37 weeks gestation). The average body mass index was 21.6 kg/m2 and the median maternal age at the beginning of pregnancy was 31 years.
Table I
Characteristics of study cohort (n = 4,800)
The results of the multiple regression analysis are presented in Table II. Listed are the coefficients that have significant variables together with their standard error and p-values. The overall adjusted R2 of the model was 0.261. The significant covariates used to model birthweight (in grams) included physiological variables (gestational age, maternal height, weight, parity, and the baby’s sex) and pathological factors (high maternal age, anaemia, smoking and pregnancy induced hypertension). The birthweight constant adjusted to 280 days was 3477.1 g for a standard mother (163 cm height, 64 kg weight, nulliparous and of baby of ‘average’, i.e. unspecified sex). Pathological effects were included within the model but not in the centile calculation. Smoking had the largest negative effect (–267.2 g). The presence of anaemia (defined as < 11.0 mg/100 ml) [21] had a positive effect on birthweight (+100.1 g).
Table II
Coefficients from multiple regression model (n = 4,270)
[i] CI – confidence interval, SE – standard error. Model is centred on the median gestational age of delivery (279 days), with coefficients expressed for a ‘standard mother’ (parity 0, maternal height 163 cm, initial weight 64 kg) and gender neutral baby. Constant (optimised by excluding all pathological factors listed): 3452.7 g, SE 372.6, CV 0.11, Adj R2 0.261.
The comparative analysis of the association of SGA on pregnancy outcome is displayed in Table III. The Fenton standard in general use identified 315 pregnancies as SGA (6.6%) and the customised standard identified 570 pregnancies (11.9%). GROW designated 278 pregnancies as SGA that were not SGA according to Fenton (‘GROW only’). This group identified additional cases in each of the 3 adverse outcome categories, all of which were significantly more at risk. The cases that were SGA by GROW only were 10 times more likely to experience a stillbirth than the general population, and all these cases were missed by the Fenton standard. Fenton designated 23 pregnancies as SGA that were not SGA by GROW, and these cases did not have increased risk of an adverse outcome.
Table III
GROW and Fenton detection of adverse outcome (n = 4,788)
[i] SGA – small for gestational age, GROW – gestation-related optimal weight, Fenton – 2013 Fenton preterm growth charts, standard, CI – confidence interval. Neonatal complication includes: intraventricular haemorrhage, transient tachypnoea, respiratory distress syndrome, hypoxic ischaemic encephalopathy, broncho-pulmonary dysplasia, sepsis or seizure.
Discussion
This is to our knowledge the first study that has created a customised birthweight standard for a Polish population.
To compare the Polish coefficients with those of other countries, we centred our regression analysis on a standard mother in her first pregnancy, with height 163 cm and weight 64 kg and delivery at a gestational age of 280 days [19]. The resultant standardised birthweight within this population was 3477.1 g (Table II). This is similar to a birthweight reference chart generated from a Polish population [22] which had a 40-week average birthweight of 3509 g. The constant is also similar to those from similarly standardised weights from other mothers of European descent: Slovenia (3451 g) [23], England (3456 g) [15], the US (3453 g) [20], Australia (3464 g) [18] and New Zealand (3464 g) [19].
The physiological variables shown to significantly affect birthweight are the same as those seen in previous analyses [8, 15, 18–20, 23, 24]; the magnitude of the effects are also comparable – for instance, the coefficient for maternal height is 6.5 g/cm and ranged from 6.4 to 9.6 g in a previous four country comparison [20]; likewise for maternal weight the coefficient is 8.5 g/kg and in the previous comparison [20] it ranged from 7.6 to 9.2 g. Pathological variables included within the regression also showed similar effects to previous analyses; for instance pregnancy induced hypertension having a –106 g effect on average birthweight [23]. Maternal age categories had a stepwise negative effect, similar to those found in the Slovenian customised standard [23], both factors being consistent with observations of increased risk of placental dysfunction in older mothers [25]. The positive effect of anaemia (+100.1 g) on birthweight seems counter to multiple studies and a systematic review that found anaemia to be a significant risk factor of low birthweight [26] A possible explanation for the increase is that these women may have received iron supplements during pregnancy, which are known to increase birthweight [27, 28].
The GROW standard calculates a 280-day term optimal weight using a mother’s height, weight, ethnicity and parity and uses a fetal proportionality curve to derive the centile lines to allow for antenatal and neonatal assessment [3]. It uses the same method to calculate fetal weight and newborn weight centiles. To compare the performance of the customised GROW standard, we tested it against the Fenton standard widely used in Poland. [16]. Fenton is a sex-specific birthweight chart that is created from multiple cohorts of pregnancy databases from Western Europe and North America and is a population-based standard, i.e. uniform for all mothers. Fenton’s lower SGA rate (6.6% vs. 11.9% with GROW) is likely to represent the fact that Polish pregnancies result in larger neonatal weights than those of West European/North American countries from which the Fenton standard was created. These differences are physiological and seen also in comparisons with other population-based standards [29–31]. Ultimately, a standard needs to relate to outcome, and as Table III shows, GROW identified as SGA many additional cases that were at increased risk of stillbirth, NICU admission and neonatal complications, while the in-use population standard by Fenton found no additional pregnancies at increased risk.
Our results add to the growing body of evidence against the use of population-based approaches to assess birthweight. The consequences of false designation as SGA could be the receipt of unnecessary treatment and diversion of resources that could be used elsewhere; while the consequences of missed SGA, as is the case with the currently used Fenton standard, are neonates not receiving the care they need in infancy.
The strength of our study was an ethnically homogeneous population with complete data for deriving customised birth weight standards, and inclusion of outcomes which allowed us to compare performance across mortality and morbidity. Variables were collected according to a standardised methodology and definitions were pre-defined.
A weakness of the study is that pathologies were often not recorded. A previous study from Poland [32] reported the smoking rate during the third trimester of pregnancy as 12%. Here, the smoking rate was 0.6% at booking, which raises questions as to ascertainment or accuracy of self reporting. The resultant effect on birthweight (Table II), of –267 g, would suggest heavy smoking according to previous models [33, 34], and because of the binary definition of smoking, we were unable to quantify the previously described dose-dependent effect related to number of cigarettes.
In conclusion, the customised standard identifies better than the Fenton growth chart neonates at increased risk of stillbirth, NICU admission and neonatal complications. False designation of SGA could result in unnecessary treatment, while missed SGA, as is the case with the currently used Fenton standard, could result in neonates not receiving adequate care they need in infancy.
Development of customised birthweight standards for a Polish population will aid clinicians caring for Polish mothers to refine the distinction between normal and abnormal small-for-gestational age fetuses [9]. The coefficients thus derived can be used to develop a country specific, individually customisable antenatal GROW tool to improve the surveillance of fetal growth in Poland.