Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CARDIOLOGY / CLINICAL RESEARCH
Concomitant multi-vessel disease is associated with
a lower procedural death rate in patients treated with
percutaneous coronary interventions within the left
main coronary artery (from the ORPKI registry)
Stanisław Bartuś
2,3
1
Department of Clinical Rehabilitation, University of Physical Education, Krakow, Poland
2
2nd Department of Cardiology and Cardiovascular Interventions, University Hospital, Krakow, Poland
3
2nd Department of Cardiology, Jagiellonian University Medical College, Krakow, Poland
4
Faculty of Medicine and Health Sciences, Jan Kochanowski University, Kielce, Poland
5
Chair of Electroradiology, Faculty of Medicine, University of Rzeszow, Rzeszow, Poland
6
Department of Interventional Cardiology, Jagiellonian University Medical College, Krakow, Poland
Submission date: 2018-04-07
Final revision date: 2018-05-31
Acceptance date: 2018-06-11
Online publication date: 2019-06-22
Publication date: 2021-07-16
Arch Med Sci 2021;17(4):881-890
KEYWORDS
percutaneous coronary interventionsleft main coronary arterymulti-vessel diseaseprocedural complicationsmortality
TOPICS
ABSTRACT
Introduction:
In this study, we aimed to distinguish differences in the procedural complication rate in a group of patients undergoing percutaneous coronary interventions (PCI) of the left main coronary artery (LMCA) between patients with isolated LMCA disease and multi-vessel disease (MVD) with LMCA involvement and to identify their predictors.
Material and methods:
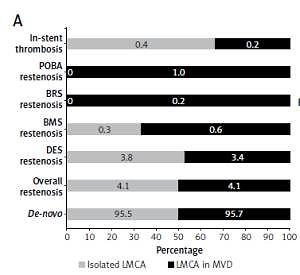
We assessed 221,187 patients from the Polish Cardiovascular Intervention Society national registry (ORPKI) regarding all PCI procedures performed in Poland in 2015 and 2016. We extracted data of 1,819 patients with isolated LMCA disease and 3,718 patients with MVD and LMCA involvement. We compared those two groups in terms of procedural complications and their predictors.
Results:
The overall rate of procedural complications was significantly higher in patients treated with LMCA PCI both in the group of patients with isolated LMCA (6.5%) and the group with MVD with LMCA involvement (7.3%) compared to the non-LMCA PCI group (1.9%, p = 0.002). Multivariate analysis confirmed that MVD with LMCA involvement is an independent predictor of decreased risk of procedural death in the overall group of patients undergoing PCI of the LMCA (odds ratio: 0.583; 95% confidence interval: 0.4–0.848; p = 0.005).
Conclusions:
The MVD involvement in patients treated with PCI of the LMCA may play a protective role. Patients with isolated LMCA involvement undergoing PCI should be subjected to special care and protected by various methods, such as devices to support left ventricle function.
In this study, we aimed to distinguish differences in the procedural complication rate in a group of patients undergoing percutaneous coronary interventions (PCI) of the left main coronary artery (LMCA) between patients with isolated LMCA disease and multi-vessel disease (MVD) with LMCA involvement and to identify their predictors.
Material and methods:
We assessed 221,187 patients from the Polish Cardiovascular Intervention Society national registry (ORPKI) regarding all PCI procedures performed in Poland in 2015 and 2016. We extracted data of 1,819 patients with isolated LMCA disease and 3,718 patients with MVD and LMCA involvement. We compared those two groups in terms of procedural complications and their predictors.
Results:
The overall rate of procedural complications was significantly higher in patients treated with LMCA PCI both in the group of patients with isolated LMCA (6.5%) and the group with MVD with LMCA involvement (7.3%) compared to the non-LMCA PCI group (1.9%, p = 0.002). Multivariate analysis confirmed that MVD with LMCA involvement is an independent predictor of decreased risk of procedural death in the overall group of patients undergoing PCI of the LMCA (odds ratio: 0.583; 95% confidence interval: 0.4–0.848; p = 0.005).
Conclusions:
The MVD involvement in patients treated with PCI of the LMCA may play a protective role. Patients with isolated LMCA involvement undergoing PCI should be subjected to special care and protected by various methods, such as devices to support left ventricle function.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.