Introduction
Breast cancer is the most common malignancy in women in Poland and in the world, and the most common cause of cancer deaths in this group of patients [1]. Advances in imaging techniques and, at the same time, their relatively high availability result in the detection of breast lesions already at the preclinical stage. However, small lesions suspected of malignancy are still a considerable diagnostic problem. Until now, the gold standard in such cases has been the open breast biopsy. However, its disadvantages, such as potential complications, the duration of the procedure, relatively high costs, scars, the extent of the surgery, and the resulting possibility of breast deformation, led to a search for less invasive and more economical methods. The techniques that eliminate or significantly reduce the above disadvantages include the vacuum-assisted biopsy (VAB) and the Breast Lesion Excision System (BLES) breast biopsy. Both methods are primarily used to excise samples for diagnostic purposes [2]. In comparison to the traditional core-needle biopsy, they provide samples of larger size, thanks to which the result of the histopathological examination is less frequently underestimated [3–6]. In some cases both methods make it possible to remove the entire lesion. What differentiates these methods is the quality for the specimen. After a VAB breast biopsy the histopathological examination of margins of a removed lesion cannot be assessed due to the fragmentation of the specimen [7]. In the BLES system, the lesion is taken in one piece, which can ensure adequate margins and intact structure of the specimen. Therefore, the BLES breast biopsy is recommended by the National Institute of Health and Clinical Excellence (NICE) as the appropriate method for removing small benign breast lesions [8]. Both of the above diagnostic methods are relatively new and not widely available; therefore they are still a subject of clinical trials. This particularly applies to the BLES system, which appeared in Poland in 2011.
The aim of the study was to compare the modern minimally invasive methods – the BLES breast biopsy and the VAB – and assess them in terms of their diagnostic and therapeutic potential.
Material and methods
The study was retrospective and involved adult patients from two oncological centers who were diagnosed and treated with one of the minimally invasive methods, the VAB or the BLES breast biopsy, between 2009 and 2016. The doctors conducting the study did not participate in the decision making process regarding the qualification of the patients for biopsy. Biopsies were performed under local anaesthesia with a 1% solution of lidocaine, in the supine position. In the case of the BLES biopsy, after anaesthesia, the skin was incised with a scalpel. In the case of the vacuum-assisted biopsy, the skin was pierced with a biopsy needle. In both techniques, the length of the skin incision was comparable (5–7 mm) and did not require stitching. To perform the VAB procedure we used the ENCOR Breast Biopsy System (Bard) with 10G or 7G needle size, for the BLES biopsy – Intact Medical Model of Elswood Group B.V. The patients who agreed to take part in the study completed the patient questionnaire 3 to 6 months after the biopsy, in which they assessed the discomfort they had experienced during the procedure, the discomfort during the days following the procedure and the final cosmetic effect. The cosmetic effect was also assessed by a surgeon in the doctor questionnaire, also filled in 3–6 months after the biopsy. Of the 173 patients who participated in the study 81 underwent the BLES breast biopsy, 88 underwent the VAB breast biopsy, and 4 patients underwent both methods. The oldest patient was 79 years old, the youngest 24, and the average age of patients participating in the study was 49. The exact characteristics of the patient group are shown in Table I.
Table I
Characteristics of the studied group
The study analyzed the data obtained from the questionnaires filled in by the patients including chronic diseases, anticoagulant and antiplatelet drugs, nicotine use, body mass index (BMI), pain associated with biopsies on an 11-point scale, subjective duration of the procedure on a 3-point scale, discomfort of the procedure on a 4-point scale, bruising after surgery on a 5-point scale, breast tenderness 24 h after biopsy on a 3-point scale, infection of the biopsy site, chronic pain and thickening in the biopsy site, the appearance of the scar on a 4-point scale, scar length on a 4-point scale, a pulling sensation of the scar, and breast deformity. Data obtained from a questionnaire filled in by a doctor – including thickening in the biopsy site, the appearance of the scar on a 4-point scale, scar length on a 4-point scale, a pulling sensation of the scar, and breast deformity – were also analyzed, as well as the data obtained from histopathological examinations.
Ethics
The study was approved by the Bioethics Committee of the Jagiellonian University (no. 122.6120.76.2015).
Statistical analysis
The Statistica 13.3 package was used for the statistical analysis. In the case of quantitative variables, due to the lack of a normal distribution of a variables, the non-parametric Mann-Whitney U test was used. In the case of qualitative variables, Pearson’s χ2 test was used. In the case of a small group size the χ2 test with the Yates correction was used. To compare the results of questions asked in both the patients and the doctors questionnaires, we used the structure ratio.
Results
In the first part of the study, the BLES breast biopsy was compared with the VAB breast biopsy in terms of the course of the procedure based on a questionnaire filled in by the patients. The patients assessed the pain experienced during the procedure on an 11-point scale (from 0 – no pain, up to 10 – unbearable pain), duration of the procedure on a 3-point scale (short, prolonged, long) and the tolerability of the procedure on a 4-point scale (neutral, unpleasant, very unpleasant, difficult to bear). Two patients were excluded from this part of the study due to incomplete questionnaires.
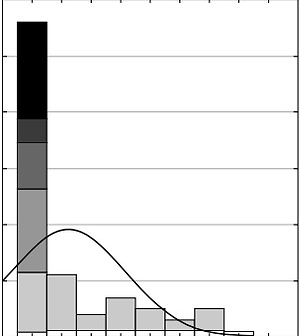
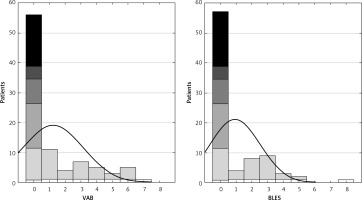
In total, the median pain score was 1. In the case of the VAB biopsy, the patients assessed the pain associated with the procedure on average at 1.22, and in the case of the BLES biopsy at 0.92 (Figure 1). However, this difference was not statistically significant (p = 0.38).
Eighty-seven percent of the patients after the VAB biopsy assessed the procedure as short, 10% as prolonged, 3% as long. In the case of the BLES biopsy, 93% of the patients rated the procedure as short, 7% as prolonged. The difference was not statistically significant (p = 0.47). None of the patients assessed the biopsy as difficult to bear. Forty-eight percent of patients after the VAB biopsy assessed the procedure as neutral, 48% as unpleasant, 4% as very unpleasant. In the case of the BLES biopsy patients, 46.5% of the patients rated the treatment as neutral, 52.5% as unpleasant, and 1% as very unpleasant. The differences were not statistically significant (p = 0.92).
Then the data about the postbiopsy period were compared. Bruising was assessed on a 5-point scale (no bruising, bruising at the biopsy site, bruising covering a breast quadrant, bruising covering more than a quadrant and less than half of the breast, bruising covering more than half of the breast), and breast tenderness approximately 24 h after the surgery was assessed on a 3-point scale (no tenderness, tenderness of the biopsy site, tenderness of the whole breast). Data about infection of the biopsy site were also collected.
There were no statistically significant differences between the groups in the case of bruising and tenderness (p = 0.07, 0.29, respectively). An infection of the biopsy site occurred only in 1 patient after a BLES biopsy.
The groups were then compared in terms of pain lasting over 3 months after a biopsy. One hundred and thirty-four patients who were not operated on after the biopsy were included in this analysis. Persistent pain occurred in 7 patients (3 after the BLES procedure, and 4 after the VAB procedure). The difference was not statistically significant (p = 0.503392).
Subsequently, the aesthetic effect was analyzed. The analysis excluded patients who were qualified for surgery after the biopsy, so only the data collected from 134 patients were used. Patients and doctors evaluated the aesthetic effect of the biopsy at least 3 months after the biopsy. The occurrence of thickening in the biopsy site (yes, no), the appearance of the scar on a 4-point scale (almost invisible, noticeable, very visible, overgrown), scar length on a 4-point scale (1–10 mm, 11–20 mm, 21–30 mm, more than 30 mm), pulling sensation of the scar (yes, no), and breast deformation (yes, no) were evaluated.
In the case of thickening at the biopsy site, pulling sensation of the scar and breast deformation assessed by the patient, the differences were not statistically significant (Table II).
Table II
Complications
| Type of complications | BLES | VAB | P-value |
|---|---|---|---|
| Thickening at the biopsy site: | 0.25140 | ||
| Yes | 4 | 6 | |
| No | 79 | 45 | |
| Pulling of the scar: | 0.73247 | ||
| Yes | 4 | 4 | |
| No | 79 | 47 | |
| Breast deformation: | 0.66662 | ||
| Yes | 1 | 2 | |
| No | 82 | 49 |
In the patients’ assessment, the scar was almost invisible or not noticeable, and none of the patient assessed the scar as very visible or overgrown. The patients after the BLES procedure assessed the scar as less visible compared to the patients after the VAB biopsy. The difference was at the edge of statistical significance (p = 0.05).
With respect to the length of the scar, the patients also marked only two responses (1–10 mm or 11–20 mm). The type of the biopsy did not influence the length of the scar (p = 0.59).
Then the data obtained from the questionnaire filled out by doctors were analyzed. The surgeons found no incident of scar pulling or breast deformity. In the case of thickening at the biopsy site, no statistically significant differences were observed (p = 0.67) between the two types of biopsies. In the case of the evaluation of the aesthetic effect of the scar and its length, none of the scars was assessed as very visible, overgrown or longer that 20 mm. In both cases, differences between groups were not statistically significant (p = 0.74 for the aesthetic effect, p = 0.1 for the length of the scar). In comparison to the answers obtained from the questionnaires filled in by the patients, there is no statistically significant difference in the assessment of the length of the scar and its aesthetic effect. However, the patients more often felt thickening at the biopsy site (p = 0.03).
Finally, the histopathological examination results were analyzed. The exact results are presented in Table III. In 1 case, after the BLES biopsy the sample was too small for a histopathological evaluation.
Table III
Histopathology results
In 54 cases of BLES samples, the margin was not assessed by a pathologist or was uncertain due to thermal damage, in 14 cases the lesion was removed without margins, and in 17 cases the lesion was removed completely with adequate margins. In 3 cases of cancers removed in the BLES, the change was removed without margins, but in one of these cases no cancer cells were found in the postoperative material. The change was completely removed more frequently in the case of fibroadenoma diagnosis compared to other histopathological diagnoses (p = 0.00002).
Discussion
The BLES breast biopsy is already considered in the literature as a tool for diagnostic and therapeutic purposes comparable to the VAB breast biopsy [7]. However, there has not been a study comparing these methods in terms of pain associated with the procedure, discomfort of the procedure, side effects and aesthetic results. Krainick-Strobel et al. found that, in the case of the VAB biopsy, the average pain score associated with the procedure on a 10-point scale was 1.35 [9]. It coincides with the results of this study, which also showed no significant difference between the VAB biopsy and the BLES biopsy in terms of pain, discomfort or duration of the procedures. Krainick-Strobel et al. as well as Liu et al. reported that the VAB biopsy was associated with a low risk of side effects, such as hematoma at the biopsy site in 5.52% of cases, which did not require a surgical intervention [9, 10]. The same results can be found in studies analyzing complications of the BLES procedure with occurrence of hematoma at the biopsy site not requiring intervention in 4.2–5.5% of cases [11–14]. Our study did not reveal any severe early or late side effects requiring intervention, either in the VAB or the BLES biopsy patients. We observed only one infection of a biopsy site after a BLES procedure. The two methods did not differ in terms of bruising and tenderness or pain lasting over 3 months after the biopsy. In the case of the aesthetic effect only Liu et al. analyzed patients’ satisfaction with the scar after the VAB procedure, and they found that about 99.52% of the patients were satisfied with the scar. In our study the patients and the doctors evaluated the aesthetic effect of the biopsy at least 3 months after the biopsy. They assessed the occurrence of thickening at the biopsy site, the appearance of the scar, scar length, pulling of the scar and breast deformation. The methods did not differ in terms of the thickening at the biopsy site, pulling of the scar, length of the scar or breast deformation assessed by the patient. However, the patients after the BLES procedure assessed the scar as less visible compared to the patients after the VAB biopsy, but the difference was at the edge of statistical significance. This difference may have been caused by the different way of inserting the needle. In the case of the BLES biopsy technique, the skin was incised with a scalpel before inserting the needle, which could lead to better healing. Nevertheless, the doctors did not see this difference. In their assessment the aesthetic effect did not differ between those two methods. What we found interesting when comparing the answers given by the patients and the doctors was that the patients more often reported thickening at the biopsy site. Taking into consideration the remodeling of the scar that may last about 1 year, the thickening felt by the patients may have been interpreted by them as a pathology while for the doctors it was part of the natural healing process [15]. In our study we did not take into consideration the preferences of the doctors performing both procedures. However, Michalopoulos et al., when analyzing the learning curve, assumed that the BLES biopsy appears to be a method easier to learn than the VAB biopsy [16]. Although there are studies showing that a lesion can be completely removed with the VAB biopsy in 72% to even 99% of cases [9, 10, 17, 18], as shown in control imaging examinations, an obvious advantage of the BLES biopsy over the VAB biopsy is the possibility to assess the margins of a lesion, which is impossible in the case of the VAB biopsy. However, in this study in 54 of the BLES samples, the margin was either not assessed by the pathologist or uncertain due to thermal damage, in 14 cases the lesion was removed without margins, and only in 17 cases was the change removed completely with adequate margins. The lesion was completely removed more frequently in the case of fibroadenoma diagnosis compared to other histopathological diagnoses. Thermal artifacts along the periphery of specimens were a problem in other studies as well [11, 19]. Al-Harethee et al. reported that thermal damage correlated with higher fat cell content of the specimen [19]. In studies where suspicious changes or verified malignant lesions were qualified for a BLES biopsy and then for surgical removal, in about 44–50% of cases there was no residual disease in the surgical samples, but only in 17–33.3% of cases was the margin of the BLES sample appropriate [13, 20–22]. In a study by Seror et al., the only independent predictive factor of a complete excision was a 1 mm margin [23]. Papanagiotou et al. suggested that a BLES biopsy allows one to remove breast cancer lesions with the diameter of 10 mm or smaller and with the appearance of a solid tumor in imaging examinations [20]. Although, theoretically, a lesion can be removed using the BLES biopsy with an appropriate margin, in many cases the margin cannot be assessed because of thermal damage. However, the thermal damage of the peripheral part of the specimen does not affect the histopathological assessment of the lesion [19]. Therefore, it appears that the BLES biopsy can be considered as a method of removing small benign and suspicious solid tumors with a subsequent surgical resection if the margins are inadequate.
The technique of the VAB biopsy does not allow one to carry out a histopathological evaluation of the degree to which the excision was radical. However, in accordance with the current recommendations, the VAB biopsy can be therapeutic for B2 lesions as well as for some B3 lesions of uncertain biological potential [24, 25].
In conclusion, there were no significant differences between the VAB breast biopsy and the BLES breast biopsy in terms of the course of the procedure, early and late complications and aesthetic effect. According to the literature, the BLES biopsy could even be easier to learn than the VAB biopsy. Since the BLES biopsy allows one to evaluate the margins of an excised lesion, it is a good alternative to the open breast biopsy and the VAB breast biopsy, without including in cases of high-risk breast lesions, assuming that with a clear 1 mm margin a surgical resection could be avoided. However, this approach requires further studies, good quality imaging examinations and good cooperation with pathologists.