The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variant B.1.1.529 was classified by the World Health Organization (WHO) as one of the variants of concern and named Omicron on November 26, 2021. The Omicron subvariant has been spreading around the world [1, 2]. It has been reported that the transmission power of the Omicron variant is 2.8 times that of the Delta variant [3]. By January 2022, BA.1 was the dominant variant circulating globally, and the BA.2 variant had been detected in several countries, including China [4, 5]. But the clinical features and severity of BA.2 in adults have not yet been well described.
The latest guidelines from the Chinese health authorities indicate that confirmed cases of SARS-CoV-2 should be treated in isolated hospitals with effective isolation and protection conditions. We describe illness severity and clinical outcomes of a 45-person China logistics cold chain-affiliated cohort from June 30, 2022 to July 21, 2022, comprising predominantly stevedores, who tested positive for BA.2. Medical staff of Qingdao Central Hospital investigated and described the epidemiologic and clinical outcomes of the cohort.
We defined illness onset as the first date a case-patient experienced any SARS-CoV-2 symptom or the specimen collection date if a person was asymptomatic. In addition, patients were classified according to their symptoms and chest computed tomography (CT) images.
We identified 45 cases; 39 (86.7%) were stevedores in the cold chain factory, while the other 6 (13.3%) were cold chain related service personal. Median age among all case-patients was 39.75 (range: 20–57) years; 44 (98%) were male (Table I). The median body mass index (BMI) of 45 patients was 25.76 kg/m2. There were 4 patients with hypertension, 2 of whom were on antihypertensive drugs before admission. Three patients had chronic hepatitis B virus infection and were not treated with anti-HBV drugs during the intervention. China has accumulated a lot of experience in prevention, diagnosis, and treatment of COVID-19. Traditional Chinese medicine (TCM) has played crucial roles in treating COVID-19 in China. During the fight against COVID-19 in China, TCM has been officially added to the diagnosis and treatment guideline issued by the National Health Commission, China [6].
Table I
Characteristics of SARS-CoV-2 Omicron BA.2 cases among cold chain-affiliated cohort, Qingdao, China, June, 2022
At least 21 (46.6%) case-patients experienced > 1 symptom, most of which were consistent with a viral upper respiratory tract infection, such as fever, sore throat, rhinorrhea and cold-like symptoms, and cough (Table I). All patients were isolated and observed in Qingdao Public Health Emergency Standby Hospital after SARS-CoV-2 PCR-positive testing, and no severe illness or death. All 45 patients were treated with integrated TCM. According to the diagnosis and treatment protocol of COVID-19 in China, a Lianhua Qingwen capsule was applied to patients with fever, and a Huoxiang Zhengqi capsule was given to patients without fever. All were cured and discharged.
Of patients cases, 45 (100%) completed the primary vaccine series, 42 (93%) received booster vaccines, 2 (4.5%) received 2 doses of vaccines, while only 1 (2.5%) received 1 dose of vaccine. None has ever suffered from SARS-CoV-2. We performed blood routine examination and chest CT for all patients. No abnormal chest imaging of any patient was found. We classified the patients according to whether they had symptoms, and divided them into asymptomatic (21 cases) and mild type patients (24 cases). There were 2 people with a low lymphocyte count (the values were 1.02 × 109/l, 1.06 × 109/l, normal value range 1.1–3.2 × 109/l), both of whom were mild type patients.
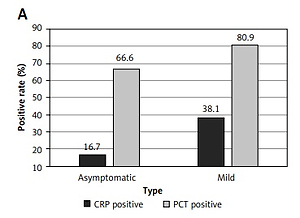
We analyzed the positive rate of CRP (C-reactive protein) and PCT (procalcitonin) in 45 patients (Figure 1 A). Compared with asymptomatic patients, mild type patients’ CRP positive rate is higher (38.1% vs. 16.7%). The PCT positive rate in mild type patients is also higher than asymptomatic patients (80.9% vs. 66.6%). From the second day of hospitalization, we carried out SARS-CoV-2 PCR testing on nasopharyngeal swabs of patients every day until discharge and analyzed the Ct value of patients during hospitalization (Figures 1 B, C). Nucleic acid of a nasopharyngeal swab with ORF1ab and N genes Ct values over 35 for 2 consecutive days (twice with an interval of at least 24 h) and length of hospital stay at least 7 days is the discharge standard of patients, according to the latest guidelines from the Chinese health authorities.
Figure 1
Characteristics of SARS-CoV-2 Omicron subvariant BA.2 in the cold chain-affiliated cohort. A – CRP and PCT positive rate in patients. B – Temporal evolution of Ct values (ORF 1ab gene). *p < 0.01, compared to the initial value; Δp < 0.05, compared to the initial value. C – Temporal evolution of Ct values (N gene).*p < 0.01, compared to the initial value; Δp < 0.05, compared to the initial value. D – Mean length of hospital stay. E – IgM antibody responses in patients. F – IgG antibody responses in patients

Compared with the initial positive value, the Ct values of ORF1ab genes in both types of patients increased significantly on the second day of hospitalization (Figure 1 B asymptomatic and mild type patients ORF1ab, 29.98 vs. 36.12, 31.54 vs. 35.21, p < 0.05). The same is true of the Ct value of the N gene (Figure 1 C asymptomatic and mild type patients N, 30.61 vs. 35.15, 31.75 vs. 34.90, p < 0.05). Although the Ct values (ORF1ab and N genes) decreased slightly on the 4th day of hospitalization, it continued to rise again on the 5th day. The mean hospital stay of asymptomatic patients was slightly longer than that of mild patients (Figures 1 D 9.16 vs. 8.62). Cold chain related person have been in a cold and humid environment for a long time, with a high moisture level and insufficient vital qi. Moisture in the body and external moisture exist at the same time, which promotes virus infection. The tongue image of all people suggests that the tongue is light and the tongue coating is greasy, which is the characteristic of a wet epidemic. According to the perspective of traditional Chinese medicine, asymptomatic people spend more time in hospital, which may be due to asymptomatic people having insufficient vital qi, their pathogenic factors are not predominant, and the struggle between vital qi and pathogenic factors is not intense.
We next compared the differences in IgM and IgG antibody values and positive rates. The IgM value of mild type patients was slightly higher than that of asymptomatic patients (Figure 1 E 0.16 vs. 0.08, p > 0.05). The same is true of IgG in mild type patients (Figure 1 F 7.53 vs. 7.30, p > 0.05). Only one patient was IgM positive, a mild type patient. Serological detection of SARS-CoV-2-specific IgG and IgM antibodies is becoming increasingly important in the management of the COVID-19 pandemic [7].
The Omicron variant of SARS-CoV-2 has rapidly replaced the Delta variant as dominating. This variant is a heavily mutated virus and designated as a variant of concern by the World Health Organization (WHO). The Omicron BA.2 variant is about 1.5 times as infectious as BA.1. It is on its path to becoming the next dominating variant.
In conclusion, 46.6% of 45 case-patients in our cohort suffered from symptomatic BA.2 infection, but all were mild and asymptomatic infections, suggesting BA.2 infection in a young population might be mild. In addition, 100% of case-patients completed a primary vaccination series which, in addition to their age, might have contributed to their mild illness. Therefore, vaccination should be encouraged. In addition, medical education on the severity of COVID-19 is also an important factor to avoid a COVID-19 pandemic [8].