Endometriosis is a common gynecological disease characterized by the presence of endometrial tissue outside the uterine cavity [1]. The impact of ovarian endometriomas’ (OE) surgery on the ovarian reserve has been widely discussed in recent years. Anti-Mullerian hormone (AMH) is the most widely used ovarian reserve marker [2]. Studies have reported that ovarian surgery has a negative impact on ovarian reserve, as evidenced by postoperative AMH levels [3]. Stage III and IV OE account for the majority of surgically treated patients. Numerous studies on OE have been published recently. However, reports comparing the characteristics of stage III and IV OE and the respective trends in AMH levels after cyst debridement are limited.
Therefore, our study focused on these issues to screen for risk factors that contribute to postoperative AMH decline and lay the groundwork for future studies to protect the ovarian reserve function in patients with OE.
Methods
General data
A prospective cohort analysis of 115 patients with OE (56 with stage III and 59 with stage IV) was conducted at the First Affiliated Hospital of Guangzhou University of Chinese Medicine, the Chinese Medicine Hospital of Hainan Province, and Guangzhou Women and Children’s Medical Center between January 2021 and January 2022. The study was approved by the Ethics Committee of Guangzhou Women and Children’s Medical Center (02701), and written informed consent was obtained from all the participants. Further information is described in supplemental materials.
Treatment methods
“Laparoscopic removal of ovarian chocolate cysts” was used for surgical treatment in both groups. After removal of the ovarian chocolate cysts, the ovarian cortex was hemostasized using sutures, because electrocoagulation was prohibited.
Statistical analysis
Statistical analysis was conducted using SPSS (version 26.0, IBM, US). The Wilcoxon nonparametric test for two correlated samples was used to compare the preoperative and postoperative AMH levels. Dichotomous logistic regression analysis was used to screen for the risk factors associated with postoperative AMH decline. Statistical significance was set at p < 0.05.
Results
Clinical characteristics and comparison of patients with stage III and IV OE
The characteristics of the patients with stage III and IV ovarian endometriomas are shown in Table I. ASRM score, preoperative CA-125, preoperative cyst volume, preoperative VAS pain score, and surgical bleeding were statistically significantly different (p < 0.05), while no significant differences were observed in other variables.
Table I
Comparison of general clinical features in patients with stage III and IV ovarian endometriosis cysts
The lateral distribution of cyst, preoperative CA-125, and cyst volume were significantly different between stage III and IV ovarian endometriomas. Notably, postoperative AMH distribution showed no significant difference between stage III and IV ovarian endometriomas (Supplementary Table SI).
Correlation analysis of CA-125, cyst volume, VAS score, and AMH
The two-variable scatter plot matrix of the four variables for the stage III and IV cases suggested no linear correlation between the variables (Supplementary Figure S1). When analyzed separately, Spearman’s rank correlation analysis revealed a correlation between CA-125 and cyst volume in both stage III and IV cases, with p-values of 0.03 and 0.01, respectively. When all cases in stages III and IV were analyzed together, Spearman’s rank correlation analysis revealed correlations between CA-125 and cyst volume as well as CA-125 and VAS pain score, with p-values of 0.000 and 0.042, respectively, and no correlations between the other variables (p > 0.05) (Supplementary Table SII).
Changes of AMH levels in patients with stage III and IV OE
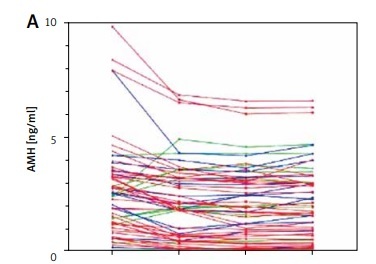
Postoperative AMH levels in patients with stage III and IV ovarian endometriomas had three manifestations – decreased, increased, and decreased – followed by an increase (Figures 1 A, B, D, E). However, overall AMH levels decreased in stages III and IV (Figures 1 C, F). The comparison between postoperative and preoperative AMH in patients with stage III and IV OE is presented in Supplementary Table SIII.
Figure 1
Postoperative AMH changes in patients with stage III and IV ovarian endometriomas. A, D – Changes in AMH in all individuals in stage III and IV cases. B, E – Changes in AMH in stage III and IV cases with lower, higher, and first lower and then higher expressions. C, F – Overall AMH changes in stage III and IV cases

Risk factors for postoperative AMH decline in patients with stage III and IV OE
The dichotomous logistic regression indicated that history of caesarean section, abortion, and preoperative CA-125 values were independent risk factors for postoperative AMH decline (Table II). The preoperative CA-125 values in the postoperative AMH decrease group differed significantly from those in the postoperative AMH decrease followed by increase group (p = 0.013) (Supplementary Figure S2).
Table II
Dichotomous logistic regression analysis of risk factors for postoperative AMH decline in patients with Stage III and IV ovarian endometriomas
Discussion
This investigation provides some information about the clinical characteristics of patients with stage III and IV ovarian endometriomas. Regarding important clinical features, stage III and IV ovarian endometriomas differed significantly. There was a correlation between CA-125 and cyst volume as well as CA-125 and VAS pain score. Although there is a general trend toward decreasing AMH levels after surgery, a different elevation may also be detected in each case. Elevated preoperative CA-125 levels, history of caesarean section, and abortion were independent risk factors for postoperative AMH decline.
AMH is the gold standard for evaluating ovarian reserve function [4]. The decrease in AMH and reduced ovarian reserve function following chocolate cyst debulking is an important clinical phenomenon that has been demonstrated in recent years [5–9], and AMH has been shown to stabilize 6 months postoperatively [8]. The results indicated an overall decreasing trend in AMH postoperatively in stage III and IV cases, which was statistically significantly different from the preoperative period, consistent with the results of other studies. Sugita et al. [5] classified the trend in postoperative AMH levels into two categories: decreasing and increasing. Based on the specific case performance in this study, it is appropriate to divide it into three categories: decreased; decreased, increased; and increased. The highest percentage of patients in this study showed a decrease postoperatively (58.93% and 64.41% in stages III and IV, respectively), followed by a decrease and increase (23.21% and 22.03% in stages III and IV). The lowest percentage showed an increase postoperatively (17.86% and 13.56% in stages III and IV), with no significant difference in the distribution of each percentage between stages III and IV.
In this study, we performed dichotomous logistic regression analysis to screen for the risk factors that contribute to postoperative AMH decline in patients with OE. The results revealed that caesarean delivery, abortion, and preoperative CA-125 were independent risk factors for postoperative AMH decline. Numerous studies have shown that an operative uterine procedure such as an abortion is a risk factor for developing endometriosis [10, 11]. This study revealed that caesarean section and abortion are risk factors for AMH decline after chocolate cyst debridement. Further studies are required to elucidate the underlying mechanisms. In addition, this study suggests that the CA-125 level is an independent risk factor for postoperative AMH decline. Combined with the finding of previous studies that CA-125 is correlated with chocolate cyst volume, we believe that the suggestive significance of CA-125 and chocolate cyst volume for postoperative AMH decline is consistent. The specific mechanism is that the higher the CA-125 level is, the larger is the volume of the chocolate cyst. This leads to the critical hypothesis that the preoperative use of GnRH-a or other progestin-like drugs to significantly reduce the volume of the chocolate cyst and lower CA-125 levels before elective surgery may be able to significantly protect ovarian reserve function. This will be further investigated in a prospective cohort study conducted by our group.
In conclusion, the clinical features showed a great difference between patients with stage III and IV ovarian endometriomas. There is a general trend toward decreasing AMH levels after surgery, but each case may also show a different elevation. CA-125 is an important biomarker for ovarian endometrioma patients, with great significance in monitoring chocolate cyst lesions.