Dilated cardiomyopathy (DCM) accounts for up to 40% of patients enrolled in clinical trials for heart failure with reduced ejection fraction, those hospitalized for heart failure, or those requiring heart transplantation [1]. To date, patients with DCM have been treated mainly with angiotensin converting enzyme inhibitors or angiotensin receptor blockers, β-blockers, mineralocorticoid receptor antagonists and SGLT2 inhibitors [2–5]. However, the pathogenesis of DCM is not fully understood and the morbidity rate remains high. Therefore, it is urgent to explore and investigate other mechanisms to provide a basis for precise prevention and treatment of DCM.
The global increase in body weight coincides with the increase in the number of people diagnosed with cardiomyopathies [6]. However, there is limited research on the correlation between body mass index (BMI) and cardiomyopathy. Wojciechowska et al. found that non-ischemic DCM patients with adverse outcomes had lower BMI values [7]. By contrast, another observational study found that BMI > 22.66 kg/m2 was strongly correlated with the recovered ejection fraction of DCM patients [8].
Mendelian randomization (MR) is a new statistical method that estimates the causal effect of modifiable exposures on outcomes through instrumental variables (IVs) [9]. Nevertheless, so far no relevant research has applied MR analysis to clarify the causal relationship between BMI and DCM. Therefore, to the best of our knowledge, we have conducted the first two-sample MR analysis to explore the potential causal relationship between BMI and DCM.
Methods
Study design
A two-sample MR analysis was conducted to assess the causal impact of BMI on DCM using SNPs as IVs. The process involved retrieving GWAS data, screening SNPs, and performing MR. In order to optimize the accuracy of the results, three key assumptions must be in place during the procedure. Assumption 1 is that genetic instrument variants are significantly associated with BMI. Assumption 2 is that the variants in the genetic instrument are clearly unrelated to the confounders. Assumption 3 is that genetic instrument variants have a strong effect on the risk of DCM via the BMI and not via other processes (Figure 1 A).
Figure 1
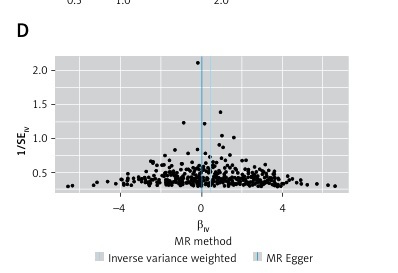
A – Design flow chart for the MR study. MR assumptions: assumptions 1, 2 and 3. Assumption 1 suggests that genetic variants correlated with BMI and affect the risk of DCM through the BMI. Assumption 2 and 3 genetic variants are not related with any confounders and do not influence the DCM through other ways. B – MR results between BMI and DCM. IVW: inverse-variance weighted. C – Scatter plots and causal estimates from three different methods. D – Funnel plots of the association of BMI and DCM

Data sources
To obtain summary data from published GWAS data on BMI and DCM, the IEU Open GWAS Project (https://gwas.mrcieu.ac.uk/) was explored. The participants were exclusively of European descent, which avoided the possibility of pleiotropic bias in cases from different ancestries [10], and the sample sizes for BMI and DCM were 461460 and 355381, respectively (Table I).
IV selection
In order to determine the IVs, we followed a two-step method. Firstly, we retrieved SNPs that are strongly related to BMI (p < 5 × 10−8). Secondly, we exclusively kept the independent SNPs, according to the linkage disequilibrium (LD) (kb = 10,000, r2 < 0.001) structure of the European population. The robustness of the IVs was assessed by calculation of the F-statistic, with a defined threshold of F > 10 for discrimination of strong IVs. IVs with an F-statistic < 10 were considered to be “weak” and were excluded from the MR analysis. To guarantee that the impact of SNP on the exposure and outcome matched the same allele, data were harmonized.
Statistical analysis
The present study used the inverse-variance weighted (IVW) method for the primary analysis. Additionally, the MR-Egger and weighted median were used as supplementary methods [11]. Sensitivity analyses were conducted to assess the reliability of the MR estimates. Heterogeneity was examined by Cochran’s Q test. The intercept in the MR-Egger method is a useful indicator of whether directional horizontal pleiotropy affects the outcomes of MR analysis. A p-value of less than 0.05 for the intercept indicates the presence of directional pleiotropy in the genetic variants. A leave-one-out sensitivity analysis was also performed to calculate the MR result of the remaining SNPs after removing the SNPs one by one [12]. The TwoSampleMR and MR-PRESSO packages in R software (version 4.2.1) were employed for all statistical analyses. Values of p < 0.05 were considered statistically significant.
Results
BMI related IV selection
According to our pre-defined filter conditions, 419 effective and independent BMI-linked SNPs were extracted as the potential IVs. Among all the selected SNPs, F-statistic values were greater than 10.
Statistical analysis
The causal relationship between BMI and DCM was found to be statistically significant in the univariable MR analysis [OR]IVW = 1.56, 95% CI: 1.26–1.92; p < 0.001). [OR] weighted median = 1.44, 95% CI: 1.03–2.01; p = 0.04), while findings from MR-Egger analysis indicated a consistent but nonsignificant direction (Figures 1 B, C).
Sensitivity analysis
The IVs selected for BMI showed no evidence of heterogeneity (MR-Egger Q statistics = 304.11, Q_df = 395, Q_pval = 0.99976; IVW Q statistics = 306.64, Q_df = 396, Q_pval = 0.99969). Moreover, MR-PRESSO detected no outlier SNPs in our sample, and the funnel plot was symmetric (Figure 1 D). No significant differences in the estimated causal effects were observed when removing individual SNPs and repeating the MR analysis in the leave-one-out analysis test.
Discussion
This study employed a two-sample MR approach to thoroughly examine the causal impact of BMI on the incidence of DCM. Our results support the positive association between genetically determined BMI and increased risk of DCM.
BMI is a widely used indicator that calculates how much a person weighs in relation to their height [13]. BMI data can be used by public health officials to develop specific strategies to tackle health problems associated with obesity, such as cardiovascular disease, type 2 diabetes and other health issues [14]. A cohort study concluded that the lowest risk of being diagnosed with cardiomyopathy was at a BMI of 21 kg/m2. The risk gradually increased with higher BMI, particularly for DCM. Severely obese subjects (BMI ≥ 35 kg/m2) had a hazard ratio of 4.71 (95% CI: 2.81–7.89) compared to those with a BMI of 20 to < 22.5 kg/m2 [15].
The mortality rate of DCM remains high, and its pathogenesis is still unclear. The possible mechanisms of BMI and obesity in DCM have not been extensively studied. A recent bioinformatics analysis study revealed that obesity disrupts the immune microenvironment, promotes oxidative stress and increases myocardial fibrosis, resulting in ventricular remodeling and an increased risk of DCM [16]. A study from the UK also suggested that DCM patients with a higher BMI show reduced efficiency of energy use. Dietary weight loss is associated with a significant improvement in myocardial contractility and a decrease in ATP delivery, suggesting improved metabolic efficiency [17]. The above studies illustrate the correlation between BMI and DCM. Basic research suggests that BMI may lead to DCM through some signaling pathways, but there has been no research on the causal relationship between BMI and DCM, which was investigated for the first time in the present study using the MR method.
In general, DCM currently lacks specific and effective treatments, and its pathogenesis remains unclear. Previous studies have suggested that obesity may contribute to the development of DCM, but the conclusions are inconsistent. BMI is a simple and convenient indicator of obesity, but there is a lack of research on the causal relationship between BMI and DCM. We performed the first two-sample MR analysis to investigate the potential causal relationship between BMI and DCM.
In conclusion, This study is the first to suggest a positive association between BMI and increased DCM risk, using a two-sample MR analysis. Our findings stress the significance of paying more attention to individuals with obesity to prevent potential DCM risk. Moreover, future studies are needed to explore the underlying mechanism mediating the causal effect of BMI on DCM.