Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
ONCOLOGY / SYSTEMATIC REVIEW/META-ANALYSIS
Cardiovascular and metabolic effects of ovarian suppression in combination with tamoxifen or an aromatase inhibitor as adjuvant therapy for early oestrogen receptor-positive breast cancer: a systematic review
1
Liverpool Centre for Cardiovascular Science at University of Liverpool, Liverpool John Moores University and Liverpool Heart & Chest Hospital, Liverpool, United Kingdom
2
School of Medicine, University of Liverpool, United Kingdom
3
Danish Center for Health Services Research, Department of Clinical Medicine, Aalborg University, Aalborg, Denmark
4
Department of Molecular and Clinical Cancer Medicine, University of Liverpool, United Kingdom
5
The Clatterbridge Cancer Centre NHS Foundation Trust, Liverpool, United Kingdom
These authors had equal contribution to this work
Submission date: 2024-02-20
Final revision date: 2024-05-17
Acceptance date: 2024-07-02
Online publication date: 2024-07-08
Corresponding author
Ying X. Gue
University of Liverpool William Henry Duncan Building 6 West Derby Street Liverpool, L7 8TX, United Kingdom
University of Liverpool William Henry Duncan Building 6 West Derby Street Liverpool, L7 8TX, United Kingdom
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Adjuvant endocrine therapy is a key treatment in oestrogen receptor positive early breast cancer (BC). For premenopausal women, ovarian function suppression (OFS) in combination with either tamoxifen or aromatase inhibitor (AI) is utilised in high-risk cases. The resultant suppression of circulating oestradiol from OFS could have adverse cardiovascular and metabolic effects, subsequently increasing the risk of cardiovascular disease.
Material and Methods:
A systematic search of online databases was conducted to identify randomised control trials involving OFS which reported cardiovascular and metabolic adverse events. Pooled odds ratios (ORs) with 95% confidence intervals (CIs) were estimated using a random-effects model.
Results:
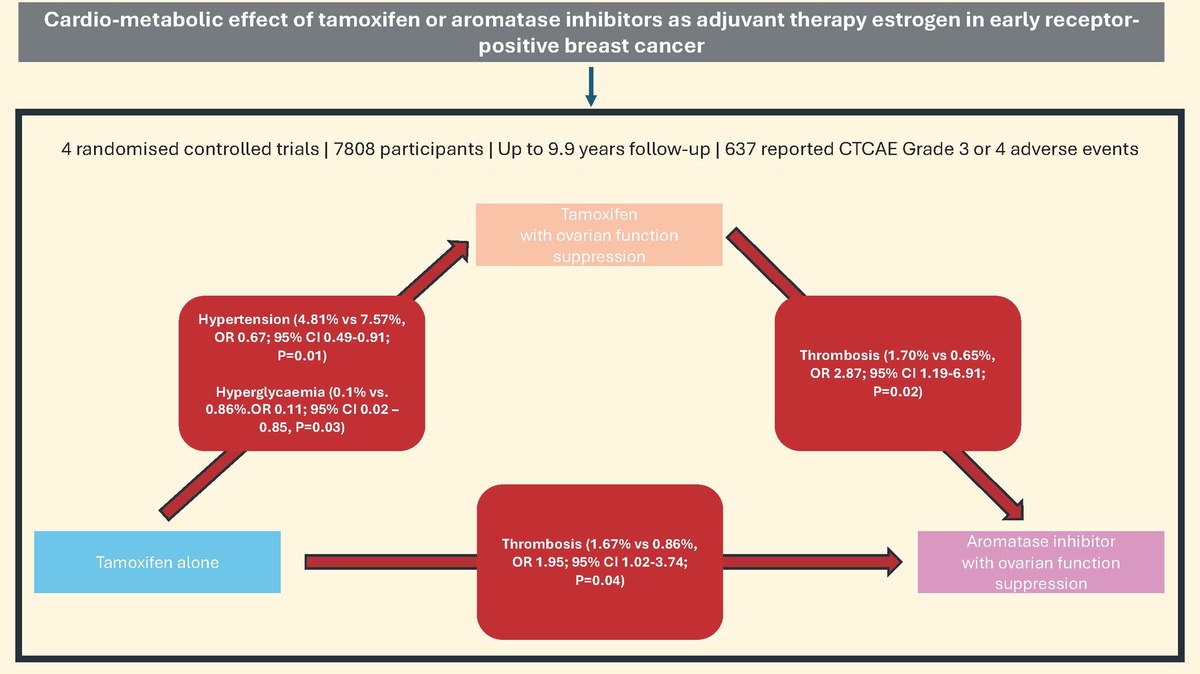
Four studies with a total of 7808 participants were included in the analysis. Tamoxifen alone carries a lower risk of hypertension compared with tamoxifen plus OFS (4.81% vs. 7.57%, OR = 0.67; 95% CI: 0.49–0.91; p = 0.01). The tamoxifen alone group showed a lower risk of hyperglycaemia compared to tamoxifen with OFS (0.10% vs. 0.86%, OR = 0.11; 95% CI: 0.02–0.85, p = 0.03).
Conclusions:
Our study highlights the potential cardio-metabolic impact of endocrine therapy and OFS on premenopausal women with BC. It also highlights the pressing need for standardisation of routine collection and recording of cardiometabolic history and risk factors as part of baseline assessment and adverse event reporting to better understand the cardiometabolic impact these treatments have on our patients. Further studies, with particular focus on baseline and subsequent development of cardiovascular risk factors, are needed to explore the impact of these drugs on the cardiovascular health of young women with BC.
Adjuvant endocrine therapy is a key treatment in oestrogen receptor positive early breast cancer (BC). For premenopausal women, ovarian function suppression (OFS) in combination with either tamoxifen or aromatase inhibitor (AI) is utilised in high-risk cases. The resultant suppression of circulating oestradiol from OFS could have adverse cardiovascular and metabolic effects, subsequently increasing the risk of cardiovascular disease.
Material and Methods:
A systematic search of online databases was conducted to identify randomised control trials involving OFS which reported cardiovascular and metabolic adverse events. Pooled odds ratios (ORs) with 95% confidence intervals (CIs) were estimated using a random-effects model.
Results:
Four studies with a total of 7808 participants were included in the analysis. Tamoxifen alone carries a lower risk of hypertension compared with tamoxifen plus OFS (4.81% vs. 7.57%, OR = 0.67; 95% CI: 0.49–0.91; p = 0.01). The tamoxifen alone group showed a lower risk of hyperglycaemia compared to tamoxifen with OFS (0.10% vs. 0.86%, OR = 0.11; 95% CI: 0.02–0.85, p = 0.03).
Conclusions:
Our study highlights the potential cardio-metabolic impact of endocrine therapy and OFS on premenopausal women with BC. It also highlights the pressing need for standardisation of routine collection and recording of cardiometabolic history and risk factors as part of baseline assessment and adverse event reporting to better understand the cardiometabolic impact these treatments have on our patients. Further studies, with particular focus on baseline and subsequent development of cardiovascular risk factors, are needed to explore the impact of these drugs on the cardiovascular health of young women with BC.
REFERENCES (21)
1.
Lumachi F, Brunello A, Maruzzo M, Basso U, Basso SM. Treatment of estrogen receptor-positive breast cancer. Curr Med Chem 2013; 20: 596-604.
2.
Paluch-Shimon S, Cardoso F, Patridge AH, et al. ESO-ESMO 4th International Consensus Guidelines for Breast Cancer in Young Women (BCY4). Ann Oncol 2020; 31: 674-96.
3.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Aromatase inhibitors versus tamoxifen in premenopausal women with oestrogen receptor-positive early-stage breast cancer treated with ovarian suppression: a patient-level meta-analysis of 7030 women from four randomised trials. Lancet Oncol 2022; 23: 382-92.
4.
Patnaik JL, Byers T, DiGuiseppi C, et al. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res 2011; 13: R64.
5.
Matthews A, Stanway S, Farmer RE, et al. Long term adjuvant endocrine therapy and risk of cardiovascular disease in female breast cancer survivors: systematic review. BMJ 2018; 363: k3845.
6.
Mendelsohn ME, Karas RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med 1999; 340: 1801-11.
7.
Martins D, Nelson K, Pan D, Tareen N, Norris K. The effect of gender on age-related blood pressure changes and the prevalence of isolated systolic hypertension among older adults: data from NHANES III. J Gend Specif Med 2001; 4: 10-3, 20.
8.
Yang G, Nowsheen S, Aziz K, Georgakilas AG. Toxicity and adverse effects of Tamoxifen and other anti-estrogen drugs. Pharmacol Ther 2013; 139: 392-404.
9.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898.
10.
Tevaarwerk AJ, Wang M, Zhao F, et al. Phase III comparison of tamoxifen versus tamoxifen plus ovarian function suppression in premenopausal women with node-negative, hormone receptor-positive breast cancer (E-3193, INT-0142): a trial of the Eastern Cooperative Oncology Group. J Clin Oncol 2014; 32: 3948-58.
11.
Francis PA, Pagani O, Fleming GD, et al. Tailoring adjuvant endocrine therapy for premenopausal breast cancer. N Engl J Med 2018; 379: 122-37.
12.
Gnant M, Mlineritsch B, H Stoeger H, et al. Zoledronic acid combined with adjuvant endocrine therapy of tamoxifen versus anastrozol plus ovarian function suppression in premenopausal early breast cancer: final analysis of the Austrian Breast and Colorectal Cancer Study Group Trial 12. Ann Oncol 2015; 26: 313-20.
13.
National Institutes of Health. Cancer Therapy Evaluation Program: common terminology criteria for adverse events, version 3.0. 2006.
14.
Honigberg MC, Zekavat SM, Aragam K, et al. Association of premature natural and surgical menopause with incident cardiovascular disease. JAMA 2019; 322: 2411-21.
15.
Wenger NK, Arnold A, Merz CNB, et al. Hypertension across a woman’s life cycle. J Am Coll Cardiol 2018; 71: 1797-1813.
16.
Kessler CM, Szymanski LM, Shamsipour Z, et al. Estrogen replacement therapy and coagulation: relationship to lipid and lipoprotein changes. Obstet Gynecol 1997; 89: 326-31.
17.
Mauvais-Jarvis F, Clegg DJ, Hevener AL. The role of estrogens in control of energy balance and glucose homeostasis. Endocr Rev 2013; 34: 309-38.
18.
Kwan ML, Cheng RK, Iribarren C, et al. Risk of cardiometabolic risk factors in women with and without a history of breast cancer: the Pathways Heart Study. J Clin Oncol 2022; 40: 1635-46.
19.
Greenlee H, Iribarren C, Rana JS, et al. Risk of cardiovascular disease in women with and without breast cancer: the Pathways Heart Study. J Clin Oncol 2022; 40: 1647-58.
20.
Bonsu JM, Guha A, Charles L, et al. Reporting of cardiovascular events in clinical trials supporting FDA approval of contemporary cancer therapies. J Am Coll Cardiol 2020; 75: 620-8.
21.
Lyon AR, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS): Developed by the task force on cardio-oncology of the European Society of Cardiology (ESC). Eur Heart J 2022; 43: 4229-361.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.