Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
METABOLIC DISORDERS / CLINICAL RESEARCH
Cardiometabolic risk in non-diabetic metabolic dysfunction-associated steatotic liver disease (MAFLD) patients: insights from the triglyceride-glucose, plasma atherogenic, and cardiometabolic index
1
Department of Gastroenterology, Erzurum Training and Research Hospital, Erzurum, Turkey
2
Department of Endocrinology and Metabolism, Erzurum Training and Research Hospital, Erzurum, Turkey
3
Department of Endocrinology and Metabolism, Sivas Numune Hospital, Sivas, Turkey
4
Department of Endocrinology and Metabolism, Rize Recep Tayyip Erdoğan University, Rize, Turkey
Submission date: 2024-06-11
Final revision date: 2024-07-01
Acceptance date: 2024-07-07
Online publication date: 2024-07-25
Corresponding author
KEYWORDS
metabolic dysfunction-associated steatotic liver diseasecardiometabolic riskcardiometabolic indextriglyceride-glucose indexplasma atherogenic index
TOPICS
ABSTRACT
Introduction:
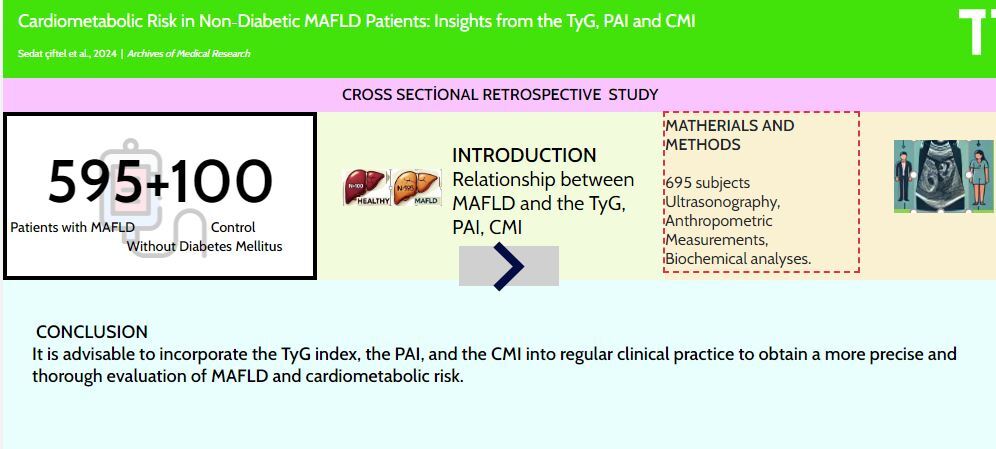
The objective of our study was to examine the correlation between hepatosteatosis and the triglyceride-glucose index (TyG), plasma atherogenic index (PAI), and cardiometabolic index (CMI) in nondiabetic patients. We also aimed to assess the usefulness of these indices in evaluating cardiometabolic risk in metabolic dysfunction-associated steatotic liver disease (MAFLD).
Material and methods:
This retrospective cross-sectional study included 695 individuals who did not have diabetes, with an average age of 39.8 ±11.3 years. A total of 595 individuals, comprising 359 women and 236 men, were diagnosed with MAFLD. The control group consisted of 100 individuals who did not have MAFLD. All the subjects underwent transabdominal ultrasonography, anthropometric measurements, and blood analyses. The groups were assessed based on the TyG index, PAI, and CMI.
Results:
TyG, PAI, and CMI were greater in patients with MAFLD than those without MAFLD. The TyG index, with a cutoff point of 8.47, excluded significant simple steatosis with a sensitivity of 65.3% and a specificity of 66.0%. The PAI and CMI cutoff values were 0.39 and 1.40, with sensitivities of 66.6% and 70.1% and specificities of 67.0% and 70.1%, respectively. The TyG index was independently associated with MAFLD (OR = 2.21, 95% CI: 1.339–3.665).
Conclusions:
The presence of MAFLD patients with a normal BMI and waist circumference indicates that these variables alone do not provide enough evidence for the diagnosis of MAFLD. Hence, it is advisable to incorporate the TyG index, the PAI, and the CMI into regular clinical practice to obtain a more precise and thorough evaluation of MAFLD and cardiometabolic risk.
The objective of our study was to examine the correlation between hepatosteatosis and the triglyceride-glucose index (TyG), plasma atherogenic index (PAI), and cardiometabolic index (CMI) in nondiabetic patients. We also aimed to assess the usefulness of these indices in evaluating cardiometabolic risk in metabolic dysfunction-associated steatotic liver disease (MAFLD).
Material and methods:
This retrospective cross-sectional study included 695 individuals who did not have diabetes, with an average age of 39.8 ±11.3 years. A total of 595 individuals, comprising 359 women and 236 men, were diagnosed with MAFLD. The control group consisted of 100 individuals who did not have MAFLD. All the subjects underwent transabdominal ultrasonography, anthropometric measurements, and blood analyses. The groups were assessed based on the TyG index, PAI, and CMI.
Results:
TyG, PAI, and CMI were greater in patients with MAFLD than those without MAFLD. The TyG index, with a cutoff point of 8.47, excluded significant simple steatosis with a sensitivity of 65.3% and a specificity of 66.0%. The PAI and CMI cutoff values were 0.39 and 1.40, with sensitivities of 66.6% and 70.1% and specificities of 67.0% and 70.1%, respectively. The TyG index was independently associated with MAFLD (OR = 2.21, 95% CI: 1.339–3.665).
Conclusions:
The presence of MAFLD patients with a normal BMI and waist circumference indicates that these variables alone do not provide enough evidence for the diagnosis of MAFLD. Hence, it is advisable to incorporate the TyG index, the PAI, and the CMI into regular clinical practice to obtain a more precise and thorough evaluation of MAFLD and cardiometabolic risk.
REFERENCES (41)
1.
Kwanten WJ. Diet and non-alcoholic fatty liver disease: a short narrative review. Acta Gastroenterol Belg 2023; 86: 306-10.
2.
Rafaqat S, Gluscevic S, Mercantepe F, Rafaqat S, Klisic A. Interleukins: pathogenesis in non-alcoholic fatty liver disease. Metabolites 2024; 14: 153.
3.
Perdomo CM, Frühbeck G, Escalada J. Impact of nutritional changes on nonalcoholic fatty liver disease. Nutrients 2019; 11: 677.
4.
Mitrovic B, Gluvic ZM, Obradovic M, et al. Nonalcoholic fatty liver disease, metabolic syndrome, and type 2 diabetes mellitus: where do we stand today? Arch Med Sci 2023; 19: 884-94.
5.
Pojsakorn D, Kanokphong S, Priyata D, et al. Disparities in metabolic dysfunction-associated steatotic liver disease and cardiometabolic conditions in low and lower middle-income countries: systematic analysis from the global burden of disease study 2019. Metabolism 2024; 155958. https://doi.org/10.1016/j.meta....
6.
Lomonaco R, Leiva EG, Bril F, et al. Advanced liver fibrosis is common in patients with type 2 diabetes followed in the outpatient setting: The need for systematic screening, Diabetes Care 2021; 44: 399-406.
7.
Harrison SA, Gawrieh S, Roberts K, et al. Prospective evaluation of the prevalence of nonalcoholic fatty liver disease and steatohepatitis in a large middle-aged US cohort. J Hepatol 2021; 75: 284-91.
8.
Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study, Gastroenterology 2011; 140: 124-31.
9.
Klisic A, Isakovic A, Kocic G, et al. Relationship between oxidative stress, inflammation and dyslipidemia with fatty liver index in patients with type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes 2018; 126: 371-8.
10.
Meneses D, Olveira A, Corripio R, et al. Performance of noninvasive liver fibrosis scores in the morbid obese patient, same scores but different thresholds. Obes Surg 2020; 30: 2538-46.
11.
Tian F, Guo Y, Zhou L, et al. Comparison of glimepiride and linagliptin in the treatment of nonalcoholic hepatic disease with type 2 diabetes mellitus. Arch Med Sci https://doi.org/10.5114/aoms/1....
12.
Borges-Canha M, Neves JS, Mendonça F, et al. The impact of bariatric surgery on hepatic function and predictors of liver steatosis and fibrosis. Obes Surg 2020; 30: 2935-41.
13.
Barton Duell P, Welty FK, Miller M, et al. Nonalcoholic fatty liver disease and cardiovascular risk: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol 2022; 42: E168-85.
14.
Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol 2020; 73: 202-9.
15.
Zhou XD, Targher G, Byrne CD, et al. An international multidisciplinary consensus statement on MAFLD and the risk of CVD. Hepatol Int 2023; 17: 773-91.
16.
Li X, Sun M, Yang Y, et al. Predictive effect of triglyceride glucose-related parameters, obesity indices, and lipid ratios for diabetes in a Chinese population: a prospective cohort study. Front Endocrinol (Lausanne) 2022; 13: 862919.
17.
Cho YK, Lee J, Kim HS, et al. Triglyceride glucose-waist circumference better predicts coronary calcium progression compared with other indices of insulin resistance: a longitudinal observational study. J Clin Med 2021; 10: 92.
18.
Dang K, Wang X, Hu J, et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003–2018, Cardiovasc Diabetol 2024; 23: 8.
19.
Irace C, Carallo C, Scavelli FB, et al. Markers of insulin resistance and carotid atherosclerosis. A comparison of the homeostasis model assessment and triglyceride glucose index. Int J Clin Pract 2013; 67: 665-72.
20.
Zhang Q, Xiao S, Jiao X, Shen Y. The triglyceride-glucose index is a predictor for cardiovascular and all-cause mortality in CVD patients with diabetes or prediabetes: evidence from NHANES 2001–2018. Cardiovasc Diabetol 2023; 22: 279.
21.
Fernández-Macías JC, Ochoa-Martínez AC, Varela-Silva JA, Pérez-Maldonado IN. Atherogenic index of plasma: novel predictive biomarker for cardiovascular illnesses. Arch Med Res 2019; 50: 285-94.
22.
Duan S, Yang D, Xia H, Ren Z, Chen J, Yao S. Cardiometabolic index: a new predictor for metabolic associated fatty liver disease in Chinese adults. Front Endocrinol (Lausanne) 2022; 13: 1004855.
23.
Wong VWS, Chan WK, Chitturi S, et al. Asia–Pacific Working Party on Nonalcoholic Fatty Liver Disease guidelines 2017 – Part 1: Definition, risk factors and assessment. J Gastroenterol Hepatol 2018; 33: 70-85.
24.
Mercantepe F, Baydur Sahin S, Cumhur Cure M, Karadag Z. Relationship between serum endocan levels and other predictors of endothelial dysfunction in obese women. Angiology 2023; 74: 948-57.
25.
Hosseini SA, Alipour M, Sarvandian S, Haghighat N, Bazyar H, Aghakhani L. Assessment of the appropriate cutoff points for anthropometric indices and their relationship with cardio-metabolic indices to predict the risk of metabolic associated fatty liver disease. BMC Endocr Disord 2024; 24: 79.
26.
Xi WF, Yang AM. Association between cardiometabolic index and controlled attenuation parameter in U.S. adults with NAFLD: findings from NHANES (2017–2020). Lipids Health Dis 2024; 23: 40.
27.
Wu Z, Xie L, Guo D, et al. Triglyceride-glucose index in the prediction of adverse cardiovascular events in patients without diabetes mellitus after coronary artery bypass grafting: a multicenter retrospective cohort study. Cardiovasc Diabetol 2023; 22: 230.
28.
Li Y, Men X, Liu Y, et al. Association with the plasma atherogenic index with hepatic steatosis and fibrosis in the US population. Medicine (United States) 2024; 103: E37152.
29.
Li XM, Liu SL, He YJ, Shu JC. Using new indices to predict metabolism dysfunction-associated fatty liver disease (MAFLD): analysis of the national health and nutrition examination survey database. BMC Gastroenterol 2024; 24: 109.
30.
Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci 2017; 13: 851-63.
31.
Arefhosseini S, Aghajani T, Tutunchi H, Ebrahimi-Mameghani M. Association of systemic inflammatory indices with anthropometric measures, metabolic factors, and liver function in nonalcoholic fatty liver disease Sci Rep 2024; 14: 12829.
32.
Jiang R, Hua Y, Hu X, Hong Z. The pan immune inflammatory value in relation to nonalcoholic fatty liver disease and hepatic fibrosis. Clin Res Hepatol Gastroenterol 2024; 48: 102393.
33.
Della Torre S. Beyond the X factor: relevance of sex hormones in nafld pathophysiology. Cells 2021; 10: 2502.
34.
Wang X, Xie J, Pang J, et al. Serum SHBG is associated with the development and regression of nonalcoholic fatty liver disease: a prospective study. J Clin Endocrinol Metab 2020; 105: 791-804.
35.
Abe RAM, Masroor A, Khorochkov A, et al. The role of vitamins in non-alcoholic fatty liver disease: a systematic review. Cureus 2021; 13: e16855.
36.
Xie C, Halegoua-Demarzio D. Role of probiotics in nonalcoholic fatty liver disease: does gut microbiota matter? Nutrients 2019; 11: 2837.
37.
Borges-Canha M, Neves JS, Silva MM, et al. Waist-to-hip ratio and inflammatory parameters are associated with risk of non-alcoholic fatty liver disease in patients with morbid obesity. Biomedicines 2022; 10: 2416.
38.
De Carli MAL, De Carli LA, Correa MB, Junqueira G, Tovo CV, Coral GP. Performance of noninvasive scores for the diagnosis of advanced liver fibrosis in morbidly obese with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol 2020; 32: 420-5.
39.
Huang CX, Zhou XD, Pan CQ, Zheng MH. Screening for metabolic dysfunction-associated fatty liver disease: time to discard the emperor’s clothes of normal liver enzymes. World J Gastroenterol 2024; 30: 2839-42.
40.
Dasarathy S, Dasarathy J, Khiyami A, Joseph R, Lopez R, Mccullough AJ, C.C. Foundation, U. States, M. Health, M. Health, U. States, C.C. Foundation, U. States, Validity of real time ultrasound in the diagnosis of hepatic steatosis: a prospective study. J Hepatol 2018; 51: 1061-7.
41.
Sumida Y, Nakajima A, Itoh Y. Limitations of liver biopsy and noninvasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol 2014; 20: 475-85.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.