Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
UROLOGY / RESEARCH PAPER
Blood count-derived inflammatory markers predict time to Bacillus Calmette-Guérin failure in high-risk non-muscle-invasive bladder cancer
1
Department of General, Oncological and Functional Urology, Medical University of Warsaw, Poland
Submission date: 2020-09-01
Final revision date: 2020-10-26
Acceptance date: 2020-11-08
Online publication date: 2021-05-05
Corresponding author
Zapała Piotr
Department of General, Oncological and Functional Urology, Medical University of Warsaw, Poland, Linleya 4, 02-005, Warsaw, Poland
Department of General, Oncological and Functional Urology, Medical University of Warsaw, Poland, Linleya 4, 02-005, Warsaw, Poland
KEYWORDS
neutrophil-to-lymphocyte rationon-muscle-invasive bladder cancerBCG failureBCG unresponsivesystemic inflammatory markers
TOPICS
ABSTRACT
Introduction:
Bacillus Calmette-Guérin (BCG) treatment failure remains a significant clinical problem in patients with high-risk non-muscle-invasive bladder cancer (NMIBC). The European Organization for Research and Treatment of Cancer (EORTC) and Spanish Urological Club for Oncological Treatment (CUETO) risk scores remain the most commonly used models in the prediction of NMIBC recurrence and progression. On the other hand, well-established predictors of BCG failure are still lacking. Our aim was to evaluate the utility of blood count-derived inflammatory markers for BCG failure prediction in patients with high-risk NMIBC.
Material and methods:
One hundred and eighty-three consecutive patients with high-risk NMIBC, who underwent transurethral resection of the bladder tumour (TURBT) and were further treated with BCG instillations were included in the study. Bacillus Calmette-Guérin failure was retrospectively determined based on European Association of Urology 2019 guidelines. Differences in BCG failure-free survival were assessed using the log-rank test. Logistic regression was utilized for uni- and multivariate analysis.
Results:
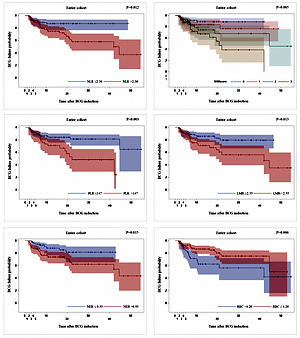
Kaplan-Meier analysis revealed that patients with a high preoperative neutrophil-to-lymphocyte ratio (NLR > 2.3), platelet-to-lymphocyte ratio (PLR > 147), neutrophil-to-erythrocyte ratio (NER > 0.93), higher systemic inflammatory marker (SIM) score and with a low lymphocyte-to-monocyte ratio (LMR < 2.55) had shorter time to BCG failure (p < 0.05). In the multivariate model, all markers except for LMR remained a significant adjunct to the CUETO recurrence risk score when predicting BCG failure.
Conclusions:
Our study demonstrates the utility of blood count-derived inflammatory markers in the prediction of BCG failure in high-risk NMIBC. Implementation of NLR, PLR, NER and SIM score might be of clinical value especially when combined with the CUETO scoring system.
Bacillus Calmette-Guérin (BCG) treatment failure remains a significant clinical problem in patients with high-risk non-muscle-invasive bladder cancer (NMIBC). The European Organization for Research and Treatment of Cancer (EORTC) and Spanish Urological Club for Oncological Treatment (CUETO) risk scores remain the most commonly used models in the prediction of NMIBC recurrence and progression. On the other hand, well-established predictors of BCG failure are still lacking. Our aim was to evaluate the utility of blood count-derived inflammatory markers for BCG failure prediction in patients with high-risk NMIBC.
Material and methods:
One hundred and eighty-three consecutive patients with high-risk NMIBC, who underwent transurethral resection of the bladder tumour (TURBT) and were further treated with BCG instillations were included in the study. Bacillus Calmette-Guérin failure was retrospectively determined based on European Association of Urology 2019 guidelines. Differences in BCG failure-free survival were assessed using the log-rank test. Logistic regression was utilized for uni- and multivariate analysis.
Results:
Kaplan-Meier analysis revealed that patients with a high preoperative neutrophil-to-lymphocyte ratio (NLR > 2.3), platelet-to-lymphocyte ratio (PLR > 147), neutrophil-to-erythrocyte ratio (NER > 0.93), higher systemic inflammatory marker (SIM) score and with a low lymphocyte-to-monocyte ratio (LMR < 2.55) had shorter time to BCG failure (p < 0.05). In the multivariate model, all markers except for LMR remained a significant adjunct to the CUETO recurrence risk score when predicting BCG failure.
Conclusions:
Our study demonstrates the utility of blood count-derived inflammatory markers in the prediction of BCG failure in high-risk NMIBC. Implementation of NLR, PLR, NER and SIM score might be of clinical value especially when combined with the CUETO scoring system.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.