Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
SYSTEMATIC REVIEW/META-ANALYSIS
Association of stress, anxiety and depression with temporomandibular disorders in young adults – a systematic review
1
King Saud University, Riyadh, Saudi Arabia
2
Bachelor of Dental Surgery, Royal College of Surgeons in Ireland, Dublin, Ireland
Submission date: 2023-07-13
Final revision date: 2023-08-22
Acceptance date: 2023-09-06
Online publication date: 2023-11-02
Publication date: 2023-11-02
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The current systematic review aims to explore whether there is an association between temporomandibular disorder (TMD) and psychological factors such as stress, anxiety, and/or depression in young adults.
Material and methods:
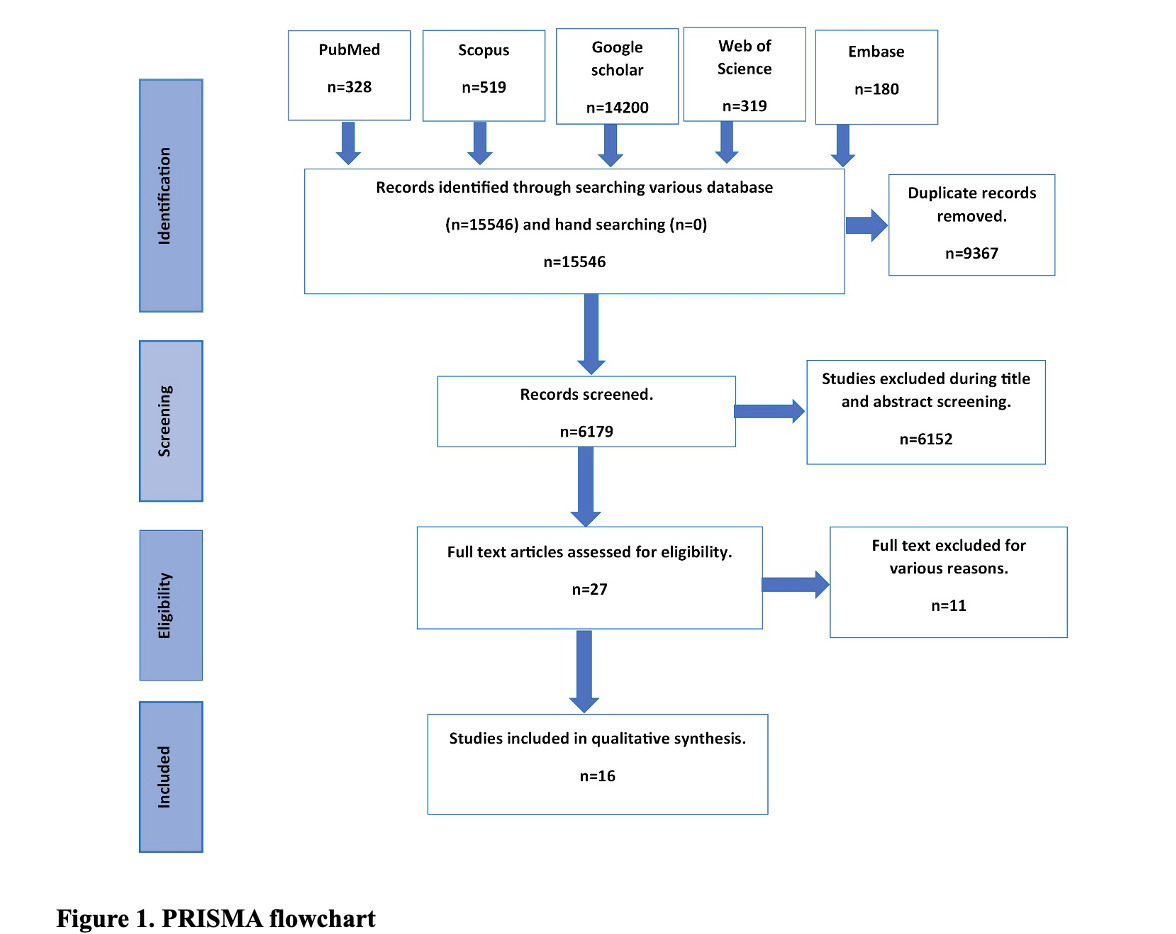
A systematic search was conducted on 14 March 2023 for publications from inception until February 2023, according to the PRISMA guidelines, using five major databases: the Cochrane Database of Systematic Reviews, PubMed, EMBASE, Web of Science, SCOPUS, and Google Scholar. The PECO framework formulated the focused question “Is there an association between TMD and psychological factors (stress/depression/anxiety) among young adults?” The study was previously registered with trial no. CRD42023407502. Articles were selected according to the inclusion criteria. For each study, risk of bias was applied to assess the quality of the included article using the Newcastle-Ottawa scoring system. The level of evidence was determined using GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) scoring.
Results:
Sixteen studies were included for final qualitative synthesis and the certainty of evidence assessment out of the 15 546 studies identified initially from different databases, with the total of 6362 participants. The included studies confirmed the association between different types of TMD and psychological factors in young adults. The risk of bias among the included studies was low, and the GRADE evidence reported was very low among included studies.
Conclusions:
Within the scope of this systematic review, it could be concluded that there is an association between temporomandibular disorder and psychological factors. Painful TMD in young females was associated with anxiety and stress.
The current systematic review aims to explore whether there is an association between temporomandibular disorder (TMD) and psychological factors such as stress, anxiety, and/or depression in young adults.
Material and methods:
A systematic search was conducted on 14 March 2023 for publications from inception until February 2023, according to the PRISMA guidelines, using five major databases: the Cochrane Database of Systematic Reviews, PubMed, EMBASE, Web of Science, SCOPUS, and Google Scholar. The PECO framework formulated the focused question “Is there an association between TMD and psychological factors (stress/depression/anxiety) among young adults?” The study was previously registered with trial no. CRD42023407502. Articles were selected according to the inclusion criteria. For each study, risk of bias was applied to assess the quality of the included article using the Newcastle-Ottawa scoring system. The level of evidence was determined using GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) scoring.
Results:
Sixteen studies were included for final qualitative synthesis and the certainty of evidence assessment out of the 15 546 studies identified initially from different databases, with the total of 6362 participants. The included studies confirmed the association between different types of TMD and psychological factors in young adults. The risk of bias among the included studies was low, and the GRADE evidence reported was very low among included studies.
Conclusions:
Within the scope of this systematic review, it could be concluded that there is an association between temporomandibular disorder and psychological factors. Painful TMD in young females was associated with anxiety and stress.
REFERENCES (52)
1.
De Leeuw R, Klasser G. Orofacial pain: guidelines for assessment, diagnosis, and management. Am J Orthod Dentofacial Orthop 2008; 134: 171.
2.
Valesan LF, Da-Cas CD, Réus JC, et al. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig 2021; 25: 441-53.
3.
Reissmann DR, John MT, Seedorf H, Doering S, Schierz O. Temporomandibular disorder pain is related to the general disposition to be anxious. J Oral Facial Pain Headache 2014; 28: 322-30.
4.
Slade G, Ohrbach R, Greenspan J, et al. Painful temporomandibular disorder: decade of discovery from OPPERA studies. J Dent Res 2016; 95: 1084-92.
5.
Sójka A, Huber J, Kaczmarek E, Hędzelek W. Ascertaining of temporomandibular disorders (TMD) with clinical and instrumental methods in the group of young adults. J Med Sci 2015; 84: 20-6.
6.
Chisnoiu AM, Picos AM, Popa S, et al. Factors involved in the etiology of temporomandibular disorders – a literature review. Clujul Med 2015; 88: 473-8.
7.
de Resende CMBM, da Silva Rocha LGD, de Paiva RP, et al. Relationship between anxiety, quality of life, and sociodemographic characteristics and temporomandibular disorder. Oral Surg Oral Med Oral Pathol Oral Radiol 2020; 129: 125-32.
8.
Helkimo M. Studies on function and dysfunction of the masticatory system: IV. Age and sex distribution of symptoms of dysfunction of the masticatory system in Lapps in the north of Finland. Acta Odontol Scand 1974; 32: 255-67.
9.
Simoen L, Van den Berghe L, Jacquet W, Marks L. Depression and anxiety levels in patients with temporomandibular disorders: comparison with the general population. Clin Oral Investig 2020; 24: 3939-45.
10.
Manfredini D, Winocur E, Ahlberg J, Guarda-Nardini L, Lobbezoo F. Psychosocial impairment in temporomandibular disorders patients. RDC/TMD axis II findings from a multicentre study. J Dent 2010; 38: 765-72.
11.
Nguyen MS, Reemann P, Loorits D, et al. Association of temporomandibular joint osseous changes with anxiety, depression, and limitation of mandibular function in elderly Vietnamese. East Asian Arch Psychiatry 2019; 29: 20-5.
12.
Riaz N. Level of depression in temporomandibular disorder patients. J Dermatol Physician Assist 2018; 27: 101-5.
13.
Akbulut A, Kurt H, Uslu Toygar H, Yıldırım E. Does anxiety have an impact on temporomandibular disorders? A study in a Turkish sample by using specific questionnaires. Cranio 2024; 42: 620-9.
14.
Aranha RLB, Martins RC, de Aguilar DR, et al. Association between stress at work and temporomandibular disorders: a systematic review. BioMed Res Int 2021; 2021: 2055513. doi: https://doi.org/10.1155/2021/2....
15.
Bonjardim LR, Gavião MBD, Pereira LJ, Castelo PM. Anxiety and depression in adolescents and their relationship with signs and symptoms of temporomandibular disorders. Int J Prosthodont 2005; 18: 347-52.
16.
Jivnani HM, Tripathi S, Shanker R, Singh BP, Agrawal KK, Singhal R. A study to determine the prevalence of temporomandibular disorders in a young adult population and its association with psychological and functional occlusal parameters. J Prosthodont 2019; 28: e445-9.
17.
Maślak-Bereś M, Loster JE, Wieczorek A, Loster BW. Evaluation of the psychoemotional status of young adults with symptoms of temporomandibular disorders. Brain Behav 2019; 9: e01443. doi: https://doi.org/10.1002/brb3.1....
18.
Reis PHF, Laxe LAC, Lacerda‐Santos R, Münchow EA. Distribution of anxiety and depression among different subtypes of temporomandibular disorder: a systematic review and meta‐analysis. J Oral Rehabil 2022; 49: 754-67.
19.
Sójka A, Stelcer B, Roy M, Mojs E, Pryliński M. Is there a relationship between psychological factors and TMD? Brain Behav 2019; 9: e01360. doi: https://doi.org/10.1002/brb3.1....
20.
Srivastava KC, Shrivastava D, Khan ZA, et al. Evaluation of temporomandibular disorders among dental students of Saudi Arabia using Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): a cross-sectional study. BMC Oral Health 2021; 21: 211.
21.
Häggman-Henrikson B, Bechara C, Pishdari B, Visscher CM, Ekberg E. Impact of catastrophizing in patients with temporomandibular disorders – a systematic review. J Oral Facial Pain Headache 2020; 34: 379-97.
22.
Zach GA, Andreasen K. Evaluation of the psychological profiles of patients with signs and symptoms of temporodiular disorders. J Prosthet Dent 1991; 66: 810-2.
23.
Alahmary AW. Association of temporomandibular disorder symptoms with anxiety and depression in Saudi dental students. Open access Macedonian journal of medical sciences. 2019;7(23):4116. doi:https://doi.org/10.3889/oamjms....
24.
Canales GT, Câmara‐Souza MB, Muñoz Lora VRM, et al. Prevalence of psychosocial impairment in temporomandibular disorder patients: a systematic review. J Oral Rehabil 2018; 45: 881-9.
25.
Uehara LM, Tardelli JDC, Botelho AL, Valente MLdC, Dos Reis AC. Association between depression and temporomandibular dysfunction in adults-a systematic review. Cranio 2023: 1-7. doi: https://doi.org/10.1080/088696....
26.
Stallman HM. Psychological distress in university students: a comparison with general population data. Aust Psychol 2010; 45: 249-57.
27.
Gonçalves DA, Dal Fabbro AL, Campos JA, Bigal ME, Speciali JG. Symptoms of temporomandibular disorders in the population: an epidemiological study. J Orofac Pain Summer 2010; 24: 270-8.
28.
Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain Fall 1999; 13: 232-7.
29.
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. doi: https://doi.org/10.1371/journa....
30.
Dubey VP, Kievišienė J, Rauckiene-Michealsson A, Norkiene S, Razbadauskas A, Agostinis-Sobrinho C. Bullying and health related quality of life among adolescents – a systematic review. Children (Basel) 2022; 9: 766.
31.
Sutherland SE. Evidence-based dentistry: Part IV. Research design and levels of evidence. J Can Dent Assoc 2001; 67: 375-8.
32.
Homeida L, Felemban E, Kassar W, Ameen M, Aldahlawi S. Temporomandibular joints disorders (TMDs) prevalence and their relation to anxiety in dental students. F1000Res 2022; 11: 271.
33.
Fernandes Azevedo AB, Câmara-Souza MB, Dantas IdS, de Resende CMBM, Barbosa GAS. Relationship between anxiety and temporomandibular disorders in dental students. Cranio 2018; 36: 300-3.
34.
Monteiro DR, Zuim PRJ, Pesqueira AA, do Prado Ribeiro P, Garcia AR. Relationship between anxiety and chronic orofacial pain of temporomandibular disorder in a group of university students. J Prosthodont Res 2011; 55: 154-8.
35.
Yap AU, Zhang MJ, Cao Y, Lei J, Fu KY. Comparison of psychological states and oral health-related quality of life of patients with differing severity of temporomandibular disorders. J Oral Rehabil 2022; 49: 177-85.
36.
Majumder K, Sharma S, Rao JKD, Siwach V, Arya V, Gulia S. Prevalence and sex distribution of temporomandibular disorder and their association with anxiety and depression in Indian medical university students. Int J Clin Med 2015; 6: 570-8.
37.
Akhter R, Murray A, Hassan N, Wickham J. Temporomandibular disorder symptoms and their association with anxiety and depression among university students. Advances in Dentistry & Oral Health 2019; 10: 1-5. doi: .https://doi.org/10.19080/ADOH.....
38.
Calixtre LB, Grüninger BLS, Chaves TC, Oliveira AB. Is there an association between anxiety/depression and temporomandibular disorders in college students? J Appl Oral Sci 2014; 22: 15-21.
39.
Reis Diniz M, Sabadin PA, Leite FP, Kamizaki R. Psychological factors related to temporomandibular disorders: an evaluation of students preparing for college entrance examinations. Acta Odontol Latinoam 2012; 25: 74-81.
40.
Arya M, Sharma S, Gupta A, et al. Incidence and clinical presentation of temporo-mandibular joint disorders and their association with psychological distress and para-functional habits in a non-patient population. J Maxillofac Oral Surg 2023; 22: 102-9.
41.
Namvar MA, Afkari BF, Moslemkhani C, Mansoori K, Dadashi M. The relationship between depression and anxiety with temporomandibular disorder symptoms in dental students. Maedica (Bucur) 2021; 16: 590-4.
42.
Yap AU, Lee DZR, Marpaung C. Negative affectivity and emotions in youths with temporomandibular disorders across cultures. Cranio 2022: 1-9. doi: https://doi.org/10.1080/088696....
43.
Cao Y, Yap AU, Lei J, Zhang MJ, Fu KY. Subtypes of acute and chronic temporomandibular disorders: their relation to psychological and sleep impairments. Oral Dis 2021; 27: 1498-506.
44.
Yap AU, Sultana R, Natu VP. Stress and emotional distress: their associations with somatic and temporomandibular disorder-related symptoms. Psychol Health Med 2022; 27: 876-87.
45.
Giannakopoulos NN, Keller L, Rammelsberg P, Kronmüller KT, Schmitter M. Anxiety and depression in patients with chronic temporomandibular pain and in controls. J Dent 2010; 38: 369-76.
46.
Saputra CM, Himawan LS, Tanti I. A study of the relationship between job related stress and temporomandibular disorders in accountants working in Jakarta. J Dent Indones 2016; 23: 69-73.
47.
Kumar SL, Naik Z, Panwar A, Sridhar M, Bagewadi A. Prevalence of temporomandibular disorders and their correlation with gender, anxiety, and depression in dental students – a cross-sectional study. JIAOMR 2022; 34: 281.
48.
McMillan A, Wong M, Lee L, Yeung R. Depression and diffuse physical symptoms in southern Chinese with temporomandibular disorders. J Oral Rehabil 2009; 36: 403-7.
49.
Canales GT, Guarda-Nardini L, Rizzatti-Barbosa CM, Conti PCR, Manfredini D. Distribution of depression, somatization and pain-related impairment in patients with chronic temporomandibular disorders. J Appl Oral Sci 2019; 27: e20180210. doi: https://doi.org/10.1590/1678-7....
50.
Zanon C, Brenner RE, Baptista MN, et al. Examining the dimensionality, reliability, and invariance of the Depression, Anxiety, and Stress Scale – 21 (DASS-21) across eight countries. Assessment 2021; 28: 1531-44.
51.
Wieckiewicz M, Jenca A, Seweryn P, et al. Determination of pain intensity, pain-related disability, anxiety, depression, and perceived stress in Polish adults with temporomandibular disorders: a prospective cohort study. Front Integr Neurosci 2022; 16: 1026781. doi: https://doi.org/10.3389/fnint.....
52.
de Santana Santos T, Pagotto LEC, Nascimento ES, da Cunha LR, Cassano DS, Gonçalves JR. Effectiveness of disk repositioning and suturing comparing open-joint versus arthroscopic techniques: a systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2021; 132: 506-13.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.