Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
DIABETOLOGY / CLINICAL RESEARCH
Association between type 1 diabetes mellitus and esophageal varices: a Mendelian randomization study
1
Thoracic Surgery Department, Binzhou People’s Hospital, Binzhou, China
2
Pharmacy Department, Binzhou People’s Hospital, Binzhou, China
3
Department of Ultrasound Medicine, Binzhou Medical University Hospital, Binzhou, China
Submission date: 2024-03-29
Final revision date: 2024-07-19
Acceptance date: 2024-07-19
Online publication date: 2024-07-25
Corresponding author
KEYWORDS
esophageal varicestype 1 diabetes mellitusMendelian randomizationmultivariate Mendelian randomization
TOPICS
ABSTRACT
Introduction:
Esophageal varices (EV) are dilated submucosal veins in the distal esophagus connecting the portal vein to the systemic circulation. Type 1 diabetes mellitus (T1DM) is a chronic autoimmune disease associated with a variety of cardiovascular and peripheral vascular diseases. The aim of this study was to investigate the causal relationship between T1DM and EV from a genetic perspective.
Material and methods:
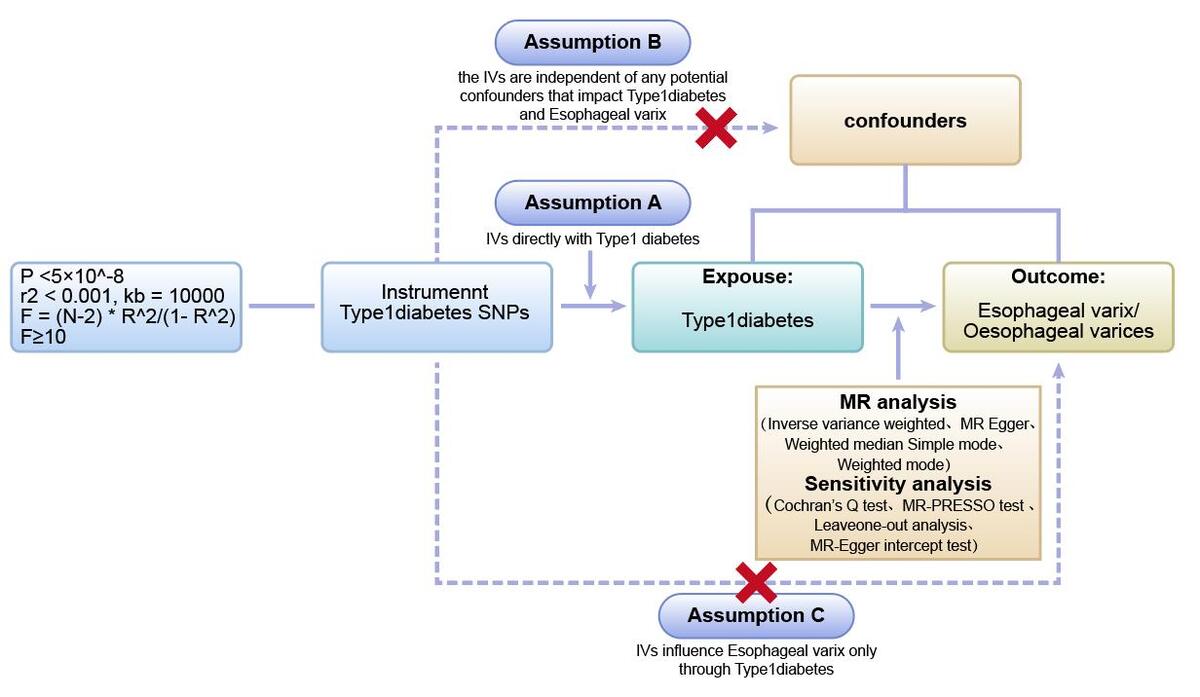
We performed a genome-wide association study of the causal relationship between T1DM and EV using pooled data from the GWAS database. Firstly, we conducted a two-sample Mendelian randomization (MR) study of these two diseases. Next, we used multivariate Mendelian randomization (MVMR) to further confirm the effect of type I diabetes on esophageal varices after excluding confounding factors such as cirrhosis and immune system disorders associated with type I diabetes mellitus. Sensitivity analyses were performed using Cochran’s Q test, MR-Egger intercept, MR Pleiotropy RESidual Sum and Outlier (MR-PRESSO) methods, leave-one-out analysis and funnel plots.
Results:
In all two-sample MR analyses, the p-values of the IVW were all < 0.05. Meanwhile, the odds ratios (ORs) of both IVW and MR-Egger analyses were > 1, and the directions of the IVW and MR-Egger assays were consistent. No horizontal pleiotropy was found for the MR-Egger intercept, and leave-one out analysis showed that the results remained stable after the removal of individual SNPs. MVMR analysis showed that the causal relationship between type I diabetes mellitus and esophageal varices persisted after exclusion of immune-related confounders.
Conclusions:
The results of the MR analysis supported a causal relationship between T1DM and EV risk.
Esophageal varices (EV) are dilated submucosal veins in the distal esophagus connecting the portal vein to the systemic circulation. Type 1 diabetes mellitus (T1DM) is a chronic autoimmune disease associated with a variety of cardiovascular and peripheral vascular diseases. The aim of this study was to investigate the causal relationship between T1DM and EV from a genetic perspective.
Material and methods:
We performed a genome-wide association study of the causal relationship between T1DM and EV using pooled data from the GWAS database. Firstly, we conducted a two-sample Mendelian randomization (MR) study of these two diseases. Next, we used multivariate Mendelian randomization (MVMR) to further confirm the effect of type I diabetes on esophageal varices after excluding confounding factors such as cirrhosis and immune system disorders associated with type I diabetes mellitus. Sensitivity analyses were performed using Cochran’s Q test, MR-Egger intercept, MR Pleiotropy RESidual Sum and Outlier (MR-PRESSO) methods, leave-one-out analysis and funnel plots.
Results:
In all two-sample MR analyses, the p-values of the IVW were all < 0.05. Meanwhile, the odds ratios (ORs) of both IVW and MR-Egger analyses were > 1, and the directions of the IVW and MR-Egger assays were consistent. No horizontal pleiotropy was found for the MR-Egger intercept, and leave-one out analysis showed that the results remained stable after the removal of individual SNPs. MVMR analysis showed that the causal relationship between type I diabetes mellitus and esophageal varices persisted after exclusion of immune-related confounders.
Conclusions:
The results of the MR analysis supported a causal relationship between T1DM and EV risk.
REFERENCES (58)
1.
Meseeha M, Attia M. Esophageal Varices. 2023 Aug 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–.
2.
Mahassadi AK, Bathaix FY, Assi C, et al. Usefulness of noninvasive predictors of oesophageal varices in Black African cirrhotic patients in Côte d’Ivoire (West Africa). Gastroenterol Res Pract 2012; 2012: 216390.
3.
Albillos A. Preventing first variceal hemorrhage in Cirrhosis. J Clin Gastroenterol 2007; 41 (Suppl 3): S305-S11.
4.
Vlachogiannakos J, Goulis J, Patch D, Burroughs AK. Review article: primary prophylaxis for portal hypertensive bleeding in cirrhosis. Aliment Pharmacol Ther 2000; 14: 851-60.
5.
Matei D, Crisan D, Procopet B, et al. Predictive factors of failure to control bleeding and 6-week mortality after variceal hemorrhage in liver cirrhosis – a tertiary referral center experience. Arch Med Sci 2022; 18: 52-61.
6.
Kim YD, Cheon GJ, Kim MY, Suk KT, Baik SK, Kim DJ. Changes in the clinical outcomes of variceal bleeding in cirrhotic patients: a 10-year experience in gangwon province, South Korea. Gut Liver 2012; 6: 476-81.
7.
Reverter E, Tandon P, Augustin S, et al. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding. Gastroenterology 2014; 146: 412-19.e3.
8.
Bambha K, Kim WR, Pedersen R, Bida JP, Kremers WK, Kamath PS. Predictors of early re-bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis. Gut 2008; 57: 814-20.
9.
Younossi ZM, Golabi P, de Avila L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol 2019; 71: 793-801.
10.
Huang DQ, Noureddin N, Ajmera V, et al. Type 2 diabetes, hepatic decompensation, and hepatocellular carcinoma in patients with non-alcoholic fatty liver disease: an individual participant-level data meta-analysis. Lancet Gastroenterol Hepatol 2023; 8: 829-36.
11.
Pennisi G, Enea M, Viganò M, et al. Oesophageal varices predict complications in compensated advanced non-alcoholic fatty liver disease. JHEP Rep 2023; 5: 100809.
12.
Jia G, Hill MA, Sowers JR. Diabetic cardiomyopathy: an update of mechanisms contributing to this clinical entity. Circ Res 2018; 122: 624-38.
13.
Joseph JJ, Deedwania P, Acharya T, et al. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation 2022; 145: e722-59.
15.
Xiong J, Hu H, Guo R, Wang H, Jiang H. Mesenchymal stem cell exosomes as a new strategy for the treatment of diabetes complications. Front Endocrinol (Lausanne) 2021; 12: 646233.
16.
Atmaca M, Ucler R, Kartal M, et al. Glycogenic hepatopathy in type 1 diabetes mellitus. Case Rep Hepatol 2015; 2015: 236143.
17.
Gregory GA, Robinson T, Linklater SE, et al. Global incidence, prevalence, and mortality of Type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabetes Endocrinol 2022; 10: 741-60.
18.
Juutilainen A, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Similarity of the impact of type 1 and type 2 diabetes on cardiovascular mortality in middle-aged subjects. Diabetes Care 2008; 31: 714-9.
19.
Standl E, Balletshofer B, Dahl B, et al. Predictors of 10-year macrovascular and overall mortality in patients with NIDDM: the Munich General Practitioner Project. Diabetologia 1996; 39: 1540-5.
20.
Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol 2003; 32: 1-22.
21.
Skrivankova VW, Richmond RC, Woolf B, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomization: the STROBE-MR Statement. JAMA 2021; 326: 1614-21.
22.
Boef AG, Dekkers OM, le Cessie S. Mendelian randomization studies: a review of the approaches used and the quality of reporting. Int J Epidemiol 2015; 44: 496-511.
23.
Burgess S, Thompson SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol 2017; 32: 377-89.
24.
Kamat MA, Blackshaw JA, Young R, et al. PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinformatics 2019; 35: 4851-3.
25.
Staley JR, Blackshaw J, Kamat MA, et al. PhenoScanner: a database of human genotype-phenotype associations. Bioinformatics 2016; 32: 3207-9.
26.
Zhang Y, Xiong Y, Shen S, et al. Causal association between tea consumption and kidney function: a Mendelian randomization study. Front Nutr 2022; 9: 801591.
27.
Pierce BL, Ahsan H, Vanderweele TJ. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int J Epidemiol 2011; 40: 740-52.
28.
Sánchez-Meca J, Marín-Martínez F. Confidence intervals for the overall effect size in random-effects meta-analysis. Psychol Methods 2008; 13: 31-48.
29.
Lee YH. Causal association between smoking behavior and the decreased risk of osteoarthritis: a Mendelian randomization. Z Rheumatol 2019; 78: 461-6.
30.
Jiang M, Ren L, Chen S, Li G. Serum uric acid levels and risk of eight site-specific cancers: a mendelian randomization study. Front Genet 2021; 12: 608311.
31.
Li C, Niu M, Guo Z, et al. A mild causal relationship between tea consumption and obesity in general population: a two-sample mendelian randomization study. Front Genet 2022; 13: 795049.
32.
Hartwig FP, Davey SG, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol 2017; 46: 1985-98.
33.
Venkatesh SS, Ferreira T, Benonisdottir S, et al. Obesity and risk of female reproductive conditions: a Mendelian randomisation study. PLoS Med 2022; 19: e1003679.
34.
Cheng F, Luk AO, Shi M, et al. Shortened leukocyte telomere length is associated with glycemic progression in type 2 diabetes: a prospective and mendelian randomization analysis. Diabetes Care 2022; 45: 701-9.
35.
Bowden J, Del GMF, Minelli C, et al. Improving the accuracy of two-sample summary-data Mendelian randomization: moving beyond the NOME assumption. Int J Epidemiol 2019; 48: 728-42.
36.
Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG. Sensitivity analyses for robust causal inference from mendelian randomization analyses with multiple genetic variants. Epidemiology 2017; 28: 30-42.
37.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 2018; 50: 693-8.
38.
Hemani G, Zheng J, Elsworth B, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife 2018; 7: e34408.
39.
Gupta TK, Chen L, Groszmann RJ. Pathophysiology of portal hypertension. Baillieres Clin Gastroenterol 1997; 11: 203-19.
41.
Sebastiani G, Tempesta D, Fattovich G, et al. Prediction of oesophageal varices in hepatic cirrhosis by simple serum non-invasive markers: results of a multicenter, large-scale study. J Hepatol 2010; 53: 630-8.
42.
Inagaki H, Nonami T, Kawagoe T, et al. Idiopathic portal hypertension associated with systemic lupus erythematosus. J Gastroenterol 2000; 35: 235-9.
43.
Yang S, Quan M, Li Y, Pan CQ, Xing H. Porto-sinusoidal vascular disease as the cause of portal hypertension in Felty’s syndrome: a case report and literature review. Biomed Res Int 2020; 2020: 2618260.
44.
Ismail AMA, El-Azeim ASA. Short-term intraocular pressure response to the combined effect of transcutaneous electrical nerve stimulation over acupoint (Acu-TENS) and yoga ocular exercise in type 2 diabetic patients with primary open-angle glaucoma: a randomized controlled trial. J Acupunct Meridian Stud 2021; 14: 193-199.
45.
Ali Ismail AM, Shaaban Abd El-Azeim A. Response of erectile dysfunction to extracorporeal shock wave therapy in type 2 diabetic men. Physiother Quart 2022; 30: 77-80.
46.
Popoviciu MS, Kaka N, Sethi Y, Patel N, Chopra H, Cavalu S. Type 1 diabetes mellitus and autoimmune diseases: a critical review of the association and the application of personalized medicine. J Pers Med 2023; 13: 422.
47.
Iwahashi A, Nakatani Y, Hirobata T, et al. Autoimmune polyglandular syndrome III in a patient with idiopathic portal hypertension. Intern Med 2013; 52: 1375-8.
48.
Takeshita Y, Takamura T, Inoue O, et al. Slowly progressive insulin-dependent diabetes in a patient with primary biliary cirrhosis with portal hypertension-type progression. Intern Med 2012; 51: 79-82.
49.
Rahmoune FC, Bruyere M, Tecsy M, Benhamou D. Alagille syndrome and pregnancy: anesthetic management for cesarean section. Int J Obstet Anesth 2011; 20: 355-8.
50.
Carr C, Desai J. OPCAB surgery in a cirrhotic hepatocellular carcinoma patient awaiting liver transplant. Ann Thorac Surg 2004; 78: 1460-2.
51.
Ford ES. Body mass index, diabetes, and C-reactive protein among U.S. adults. Diabetes Care 1999; 22: 1971-7.
52.
Hayaishi-Okano R, Yamasaki Y, Katakami N, et al. Elevated C-reactive protein associates with early-stage carotid atherosclerosis in young subjects with type 1 diabetes. Diabetes Care 2002; 25: 1432-8.
53.
Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation 2008; 117: 93-102.
54.
Peng YH, Lin YS, Chen CH, et al. Type 1 diabetes is associated with an increased risk of venous thromboembolism: a retrospective population-based cohort study. PLoS One 2020; 15: e0226997.
55.
Toplak H, Stauber R, Sourij H. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease: guidelines, clinical reality and health economic aspects. Diabetologia 2016; 59: 1148-9.
56.
Harman DJ, Kaye PV, Harris R, Suzuki A, Gazis A, Aithal GP. Prevalence and natural history of histologically proven chronic liver disease in a longitudinal cohort of patients with Type 1 diabetes. Hepatology 2014; 60: 158-68.
57.
Shen J, Wang Y, Zhou S, et al. Lung function and nonalcoholic fatty liver disease: a Mendelian randomization study. Arch Med Sci 2025; 21: 197-205.
58.
Mazidi M, Shekoohi N, Katsiki N, Banach M. Omega-6 fatty acids and the risk of cardiovascular disease: insights from a systematic review and meta-analysis of randomized controlled trials and a Mendelian randomization study. Arch Med Sci 2022; 18: 466-79.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.