Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CARDIOLOGY / CLINICAL RESEARCH
Association between Life’s Essential 8 and depression: a population-based study
1
Zhejiang Chinese Medical University, Hangzhou, China
2
Department of Psychiatry, Huzhou Third Municipal Hospital, the Affiliated Hospital of Huzhou University, Huzhou, China
Submission date: 2024-03-14
Final revision date: 2024-07-06
Acceptance date: 2024-07-15
Online publication date: 2024-07-25
Corresponding author
Haizhi Chen
Huzhou Third Municipal Hospital, the Affiliated Hospital of Huzhou University, HuZhou, China
Huzhou Third Municipal Hospital, the Affiliated Hospital of Huzhou University, HuZhou, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Previous research has established a connection between depression and an elevated risk of cardiovascular disease. In this study, we sought to examine the association between Life’s Essential 8 (LE8), an updated metric for assessing cardiovascular health, and the prevalence and severity of depressive symptoms.
Material and methods:
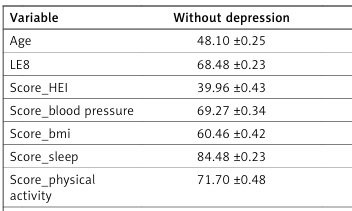
This investigation draws on data from 29 100 participants in the 2005-2018 National Health and Nutrition Examination Survey. LE8 was determined by eight metrics (diet, physical activity (PA), nicotine exposure, sleep quality, body mass index, blood lipid levels, blood glucose, and blood pressure (BP)), and was characterized as low, moderate, and high cardiovascular health (CVH). We examined the association between LE8 scores and depression using multivariate logistic regression, adjusting for a range of sociodemographic, lifestyle, and health-related variables.
Results:
Higher LE8 scores and CVH levels were associated with lower odds of depression. Each additional LE8 point correlated with 5% lower odds of depression (p < 0.05). Participants with low CVH had over 8-fold higher odds of depression compared to those with high CVH (p < 0.05). Those with moderate CVH had around 3-fold higher odds versus high CVH (p < 0.05). These associations persisted after adjustment for sociodemographics, health behaviors, and clinical variables. A higher LE8 displayed a negative association with all-cause mortality (HR = 0.975, 95% CI: 0.972, 0.978, p < 0.0001) and cardiovascular mortality (HR = 0.987, 95% CI: 0.981,0.993, p < 0.0001).
Conclusions:
Higher adherence to LE8 lifestyle recommendations was associated with lower odds of depression in a nationally representative sample. Promoting LE8 may be an effective public health strategy to prevent depression.
Previous research has established a connection between depression and an elevated risk of cardiovascular disease. In this study, we sought to examine the association between Life’s Essential 8 (LE8), an updated metric for assessing cardiovascular health, and the prevalence and severity of depressive symptoms.
Material and methods:
This investigation draws on data from 29 100 participants in the 2005-2018 National Health and Nutrition Examination Survey. LE8 was determined by eight metrics (diet, physical activity (PA), nicotine exposure, sleep quality, body mass index, blood lipid levels, blood glucose, and blood pressure (BP)), and was characterized as low, moderate, and high cardiovascular health (CVH). We examined the association between LE8 scores and depression using multivariate logistic regression, adjusting for a range of sociodemographic, lifestyle, and health-related variables.
Results:
Higher LE8 scores and CVH levels were associated with lower odds of depression. Each additional LE8 point correlated with 5% lower odds of depression (p < 0.05). Participants with low CVH had over 8-fold higher odds of depression compared to those with high CVH (p < 0.05). Those with moderate CVH had around 3-fold higher odds versus high CVH (p < 0.05). These associations persisted after adjustment for sociodemographics, health behaviors, and clinical variables. A higher LE8 displayed a negative association with all-cause mortality (HR = 0.975, 95% CI: 0.972, 0.978, p < 0.0001) and cardiovascular mortality (HR = 0.987, 95% CI: 0.981,0.993, p < 0.0001).
Conclusions:
Higher adherence to LE8 lifestyle recommendations was associated with lower odds of depression in a nationally representative sample. Promoting LE8 may be an effective public health strategy to prevent depression.
REFERENCES (31)
1.
Zhou B, Zhu Z, Ransom BR, et al. Oligodendrocyte lineage cells and depression. Mol Psychiatry 2021; 26: 103-17.
2.
Furukawa TA, Cipriani A, Cowen PJ, et al. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry 2019; 6: 601-9.
3.
Pan A, Sun Q, Okereke OI, et al. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA 2011; 306: 1241-9.
4.
Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010; 121: 586-613.
5.
Lloyd-Jones DM, Ning H, Labarthe D, et al. Status of Cardiovascular Health in US Adults and Children Using the American Heart Association’s New “Life’s Essential 8” Metrics: Prevalence Estimates From the National Health and Nutrition Examination Survey (NHANES), 2013 Through 2018. Circulation 2022; 146: 822-35.
6.
Cao Z, Yang H, Ye Y, et al. Polygenic risk score, healthy lifestyles, and risk of incident depression. Transl Psychiatry 2021; 11: 189.
7.
Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA 2021; 326: 1-13.
8.
Li Z, Wang W, Xin X, et al. Association of total zinc, iron, copper and selenium intakes with depression in the US adults. J Affect Disord 2018; 228: 68-74.
9.
Li X, Liu H, Zhang L, et al. Association between dietary theobromine with depression: a population-based study. BMC Psychiatry 2022; 22: 769.
10.
Chen H, Tang H, Huang J, et al. Life’s Essential 8 and mortality in US Adults with chronic kidney disease Am J Nephrol 2023; 54: 516-27.
11.
Kant AK, Graubard BI. A comparison of three dietary pattern indexes for predicting biomarkers of diet and disease. J Am Coll Nutr 2005; 24: 294-303.
12.
Lloyd-Jones DM, Allen NB, Anderson CAM, et al. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: a presidential advisory from the American Heart Association. Circulation 2022; 146: e18-43.
13.
Buerger A, Emser T, Seidel A, et al. DUDE – a universal prevention program for non-suicidal self-injurious behavior in adolescence based on effective emotion regulation: study protocol of a cluster-randomized controlled trial. Trials 2022; 23: 97.
14.
Flint KM, Fairclough DL, Spertus JA, et al. Does heart failure-specific health status identify patients with bothersome symptoms, depression, anxiety, and/or poorer spiritual well-being? Eur Heart J 2019; 5: 233-41.
15.
Gao L, Ge W, Peng C, et al. Association between dietary theobromine and cognitive function in a representative american population: a cross-sectional study. J Prev Alzheimer’s Dis 2022; 9: 449-57.
16.
Kim K, Song Y, Oh TJ, et al. Association between iron intake and diabetic peripheral neuropathy in type 2 diabetes: significance of iron intake and the ratio between iron intake and polyunsaturated fatty acids intake Nutrients 2020; 12: 3365.
17.
Rattan P, Penrice DD, Ahn JC, et al. Inverse association of telomere length with liver disease and mortality in the US population. Hepatol Commun 2022; 6: 399-410.
18.
Perng W, Aris IM, Slopen N, et al. Application of Life’s Essential 8 to assess cardiovascular health during early childhood. Ann Epidemiol 2023; 80: 16-24.
19.
Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch General Psychiatry 2010; 67: 220-9.
20.
Milaneschi Y, Simmons WK, van Rossum EFC, et al. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry 2019; 24: 18-33.
21.
Pérez-Pérez A, Sánchez-Jiménez F, Maymó J, et al. Role of leptin in female reproduction. Clin Chem Labor Med 2015; 53: 15-28.
22.
Bornstein SR, Schuppenies A, Wong M, et al. Approaching the shared biology of obesity and depression: the stress axis as the locus of gene-environment interactions. Mol Psychiatry 2006; 11: 892-902.
23.
Fabricatore AN, Wadden TA, Higginbotham AJ, et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes 2011; 35: 1363-76.
24.
Leonard BE. Inflammation and depression: a causal or coincidental link to the pathophysiology? Acta Neuropsychiatr 2018; 30: 1-16.
25.
Muhammad HFL, Vink RG, Roumans NJT, et al. Dietary intake after weight loss and the risk of weight regain: macronutrient composition and inflammatory properties of the diet. Nutrients 2017; 9: 1205.
26.
Paulson D, Lichtenberg PA. Vascular depression and frailty: a compound threat to longevity among older-old women. Aging Mental Health 2013; 17: 901-10.
27.
Jeter PE, Slutsky J, Singh N, et al. Yoga as a Therapeutic intervention: a bibliometric analysis of published research studies from 1967 to 2013. J Altern Complement Med 2015; 21: 586-92.
28.
Wu Y, Huang X, Bell C, et al. Ginsenoside Rb1 improves leptin sensitivity in the prefrontal cortex in obese mice. CNS Neurosci Ther 2018; 24: 98-107.
29.
Marin Bosch B, Bringard A, Logrieco MG, et al. A single session of moderate intensity exercise influences memory, endocannabinoids and brain derived neurotrophic factor levels in men. Sci Rep 2021; 11: 14371.
30.
Jacka FN, O’Neil A, Opie R, et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med 2017; 15: 23.
31.
Parletta N, Zarnowiecki D, Cho J, et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: a randomized controlled trial (HELFIMED). Nutr Neurosci 2019; 22: 474-87.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.