Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
NUTRITION / CLINICAL RESEARCH
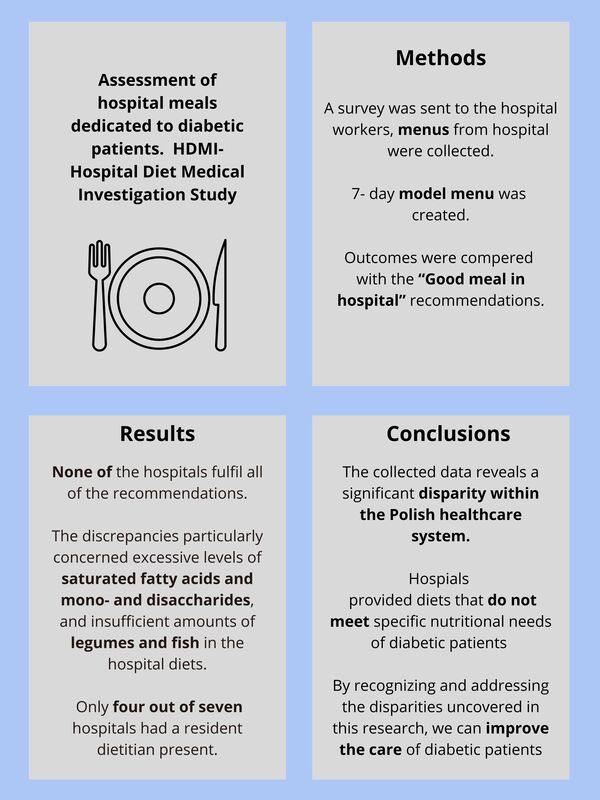
Assessment of special hospital meals for diabetic patients. Discrepancies between provided meals, model menus and dietary guidelines: a hospital diet medical investigation (HDMI) study
1
3rd Department of Internal Medicine and Cardiology, Medical University of Warsaw, Warsaw, Poland
2
Department of Human Nutrition, Medical University of Warsaw, Warsaw, Poland
3
Department of Education and Research in Health Sciences, Medical University of Warsaw, Warsaw, Poland, Poland
4
Polish Society of Lifestyle Medicine, Warsaw, Poland
5
Department of Internal Medicine, Rehabilitation and Physical Medicine, Medical University of Lodz, Lodz, Poland
6
Department of Heart Failure and Cardiac Rehabilitation, Medical University of Warsaw, Warsaw, Poland
Submission date: 2024-05-06
Final revision date: 2024-07-15
Acceptance date: 2024-07-16
Online publication date: 2024-08-06
Corresponding author
Alicja M. Jodczyk
3rd Department of Internal Medicine and Cardiology, Medical University of Warsaw, Warsaw, Poland, warsaw, Poland
3rd Department of Internal Medicine and Cardiology, Medical University of Warsaw, Warsaw, Poland, warsaw, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
In Poland, it is estimated that more than 2 million individuals have diabetes. Intervening in modifiable risk factors can effectively prevent and delay the onset of type 2 diabetes. Previous reports claimed that the Polish healthcare system did not guarantee proper nutrition and nutritional education. This study aimed to examine the dietary provisions for diabetic patients in Poland’s hospitals and evaluate their compliance with the Good Meal in Hospital (Dobry Posiłek w Szpitalu) guidelines.
Material and methods:
Hospital workers were asked to complete the survey regarding hospital (degree of reference, number of beds in total and internal medicine unit, availability of a special diet for diabetic patients, performing nutritional education and presence of a dietitian) and attach menus from meals received by patients from 10 consecutive days. The menus were analyzed in a computer program for assessment of institutional nutrition and then compared to a self-made model menu and the Good Meal in Hospital guidelines. These are the first such recommendations in Poland that introduce a coherent system to plan meals in hospitals. For each nutritional value, the mean (M), standard deviation (SD), and range (min–max.) were calculated. To assess differences in means for nutrients and products a one-way analysis of variance (ANOVA) followed by Dunnett’s two-tailed test was used.
Results:
Seventy menus from seven hospitals were examined. Five hospitals met eight and two hospitals met seven out of thirteen criteria. The discrepancies particularly concerned excessive levels of saturated fatty acids and mono- and disaccharides, and insufficient amounts of legumes and fish in the hospital diets. Only four out of seven hospitals had a resident dietitian present.
Conclusions:
Providing meals containing typical nutritional errors representing the pattern of the Polish population during hospitalization may lead to potential post-discharge dietary errors. They may result in deterioration in glycemic regulation and lipid profiles, and heightened susceptibility to complications, including elevated cardiovascular risk.
In Poland, it is estimated that more than 2 million individuals have diabetes. Intervening in modifiable risk factors can effectively prevent and delay the onset of type 2 diabetes. Previous reports claimed that the Polish healthcare system did not guarantee proper nutrition and nutritional education. This study aimed to examine the dietary provisions for diabetic patients in Poland’s hospitals and evaluate their compliance with the Good Meal in Hospital (Dobry Posiłek w Szpitalu) guidelines.
Material and methods:
Hospital workers were asked to complete the survey regarding hospital (degree of reference, number of beds in total and internal medicine unit, availability of a special diet for diabetic patients, performing nutritional education and presence of a dietitian) and attach menus from meals received by patients from 10 consecutive days. The menus were analyzed in a computer program for assessment of institutional nutrition and then compared to a self-made model menu and the Good Meal in Hospital guidelines. These are the first such recommendations in Poland that introduce a coherent system to plan meals in hospitals. For each nutritional value, the mean (M), standard deviation (SD), and range (min–max.) were calculated. To assess differences in means for nutrients and products a one-way analysis of variance (ANOVA) followed by Dunnett’s two-tailed test was used.
Results:
Seventy menus from seven hospitals were examined. Five hospitals met eight and two hospitals met seven out of thirteen criteria. The discrepancies particularly concerned excessive levels of saturated fatty acids and mono- and disaccharides, and insufficient amounts of legumes and fish in the hospital diets. Only four out of seven hospitals had a resident dietitian present.
Conclusions:
Providing meals containing typical nutritional errors representing the pattern of the Polish population during hospitalization may lead to potential post-discharge dietary errors. They may result in deterioration in glycemic regulation and lipid profiles, and heightened susceptibility to complications, including elevated cardiovascular risk.
REFERENCES (32)
1.
International Diabetes Federation. IDF Diabetes Atlas 2021- 10th edition. Published 2021. Accessed November 21, 2023. https://diabetesatlas.org/.
2.
Ministry of Health. Diabetes. Published December 14, 2022. Accessed November 21, 2023. https://archiwum.mz.gov.pl/zdr....
3.
de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 1999; 99: 779-85.
4.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure [published correction appears in Eur Heart J 2021; 42: 4901]. Eur Heart J 2021; 42: 3599-726.
5.
Diabetes in America. 3rd edn. Ley SH, Schulze MB, Hivert MF, et al. (eds.) National Institute of Diabetes and Digestive and Kidney Diseases (US), Bethesda (MD) 2018.
6.
Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 2014; 383: 1999-2007.
7.
Cicero AFG, Fogacci F. The year in nutrition medicine 2023. Arch Med Sci 2023; 19: 1599-1601.
8.
Liu D, Shi Q, Cheng G, Huang Q, Li S. Worldwide burden attributable to diet high in red meat from 1990 to 2019. Arch Med Sci 2022; 19: 1-15.
9.
Liese AD, Nichols M, Sun X, D’Agostino RB Jr, Haffner SM. Adherence to the DASH Diet is inversely associated with incidence of type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes Care 2009; 32: 1434-6.
10.
Salas-Salvadó J, Bulló M, Estruch R, et al. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial [published correction appears in Ann Intern Med 2018; 169: 271-2]. Ann Intern Med 2014; 160: 1-10.
11.
Tonstad S, Stewart K, Oda K, Batech M, Herring RP, Fraser GE. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr Metab Cardiovasc Dis 2013; 23: 292-9.
12.
Araszkiewicz A, Bandurska-Stankiewicz E, Borys S, et al. 2023 Guidelines on the management of patients with diabetes – a position of Diabetes Poland. Curr Topics Diabetes 2023; 3: 1-133.
13.
Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. J Acad Nutr Diet 2015; 115: 1323-34.
14.
NIK – The Supreme Audit Office Nutrition of Patients in Hospitals. Published April 13, 2018. Accessed November 10, 2023. https://www.nik.gov.pl/aktualn....
15.
prof. MUDr. Roman Havlík, Ph.D., ředitel Fakultní nemocnice Olomouc. Projekt Nemocniční strava. Published February 27, 2019. Accessed June 29, 2024.: https://www.nemocnicnistrava.c...
16.
Dr. Kristin Hünninghaus, Prof. Dr. Gustav Dobos, Dr. Markus Keller , et al. Offener Brief: Ernährung im Krankenhaus – wichtig für Gesundheit und Umwelt. Accessed June 29, 2024. https://pan-int.org/de/ernaehr....
17.
Ministry of Health. Good meal in the hospital. Published September 27, 2023. Accessed November 21, 2023. https://www.gov.pl/web/zdrowie....
18.
Sińska B, Kucharska A. Dietary guidelines in diabetes – why are they so difficult to follow? Zalecenia żywieniowe w cukrzycy – dlaczego tak trudno ich przestrzegać? Pediatr Endocrinol Diabetes Metab 2023; 29: 125-7.
19.
ElSayed NA, Aleppo G, Aroda VR, et al. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes-2023. Diabetes Care 2023; 46 (Suppl 1): S68-96.
20.
Asche C, LaFleur J, Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther 2011; 33: 74-109.
21.
Czapla M, Juárez-Vela R, Łokieć K, Wleklik M, Karniej P, Smereka J. The association between nutritional status and length of hospital stay among patients with hypertension. Int J Environ Res Public Health 2022; 19: 5827.
22.
Zaremba N, Watson A, Kan C, et al. Multidisciplinary healthcare teams’ challenges and strategies in supporting people with type 1 diabetes to recover from disordered eating. Diabet Med 2020; 37: 1992-2000.
23.
American Diabetes Association Professional Practice Committee. 3. Prevention or Delay of Diabetes and Associated Comorbidities: Standards of Care in Diabetes-2024. Diabetes Care 2024; 47 (Suppl 1): S43-51.
24.
Beverly EA, Ganda OP, Ritholz MD, et al. Look who’s (not) talking: diabetic patients’ willingness to discuss self-care with physicians. Diabetes Care 2012; 35: 1466-72.
25.
Heisler M, Cole I, Weir D, Kerr EA, Hayward RA. Does physician communication influence older patients’ diabetes self-management and glycemic control? Results from the Health and Retirement Study (HRS). J Gerontol A Biol Sci Med Sci 2007; 62: 1435-42.
26.
National Center for Nutrition Education. National survey of the diet and nutritional status of the Polish population – report 2021. Published October 26, 2021. Accessed December 6, 2023. Available online: https://ncez.pzh.gov.pl/sdm_do....
27.
Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014; 37 Suppl 1: S120-43.
28.
He M, van Dam RM, Rimm E, Hu FB, Qi L. Whole-grain, cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation 2010; 121: 2162-8.
29.
Burger KN, Beulens JW, van der Schouw YT, et al. Dietary fiber, carbohydrate quality and quantity, and mortality risk of individuals with diabetes mellitus. PLoS One 2012; 7: e43127.
30.
Zafar MI, Mills KE, Zheng J, et al. Low-glycemic index diets as an intervention for diabetes: a systematic review and meta-analysis. Am J Clin Nutr 2019; 110: 891-902.
31.
Schwingshackl L, Strasser B, Hoffmann G. Effects of monounsaturated fatty acids on glycaemic control in patients with abnormal glucose metabolism: a systematic review and meta-analysis. Ann Nutr Metab 2011; 58: 290-6.
32.
Rożdżeński W. improper nutrition as a basis of responsibilty of a medical entity. Med Law Quart 2019; 2: 71-98. https://przegladprawamedyczneg....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.