Coronary artery disease (CAD) remains the third cause of death among individuals aged ≥ 35 years globally [1]. Patient-reported treatment burden (TBN) refers to the patient’s time and effort invested in the management of their chronic health conditions and the impact of that effort on their overall functioning and well-being [2]. High TBN is associated with various unfavourable outcomes, such as non-adherence, higher hospitalisation rates, exacerbation of chronic health conditions, and higher mortality [3, 4]. It has been shown that TBN of ≥ 59 points, as assessed using the Treatment Burden Questionnaire (TBNQ), is indicative of an unacceptably high TBN for patients [5]. We have previously reported that patients with atrial fibrillation (AF) had a significantly higher TBN in comparison to those without AF [6]. In addition, we found that female patients with AF might experience a higher TBN compared to male patients [7], and observed that CAD was a positive predictor of a higher TBN in AF patients, especially in females [6, 7]. A possible explanation could be the fact that when cardiovascular disease is revealed the prognosis is significantly worse in females compared to males [8]. Nevertheless, data are lacking regarding specific features of TBN in patients with CAD. In this exploratory analysis we aimed to address this research gap by exploring and characterising TBN in patients with CAD.
Methods
The rationale and design of the study have been previously reported [6, 7]. Briefly, consecutive adult patients were invited to voluntarily fill out the study questionnaires during the enrolment period from April to June 2019, during their clinical visit to the University Clinical Centre of Serbia. Only patients who had been taking therapy for one or more chronic medical conditions for a minimum of 6 months before enrolment in this study were eligible for inclusion in the research. The TBN questionnaire has been developed and validated for assessing TBN in patients undergoing treatment for various chronic health conditions and cardiovascular diseases [9]. The TBN questionnaire comprises 13 items that examine the burden associated with taking medicine, self-monitoring, organisational and administrative requirements, following medical advice regarding diet and physical activity, as well as the social repercussions of the treatment. The question regarding the financial burden of treatment was excluded from the questionnaire due to the availability of a comprehensive national public health insurance programme for all Serbian citizens. In addition, participants completed the EQ-5D questionnaire.
Statistical analysis
Continuous variables were expressed as means with standard deviations (SD) and analysed using Students’ t-test, while categorical variables were presented as frequencies and corresponding percentages and analysed using the χ2 test.
The TBNQ score represents the sum of the points assigned by patients to each question, ranging from 1 (indicating minimal burden) to 10 (reflecting the highest burden). The response “I don’t know” to questions and unanswered questions were assigned 0 points, signifying the absence of perceived burden for the patient. The TBNQ score ranged from 0 to 170 points.
The TBNQ score was analysed as a continuous variable using linear regression analysis and presented as the standard coefficient β with a corresponding 95% confidence interval (CI). Moreover, the TBNQ score was stratified into quartiles, with the lowest quartile defined as TBNQ of ≤ 26 points and the highest quartile as TBNQ of ≥ 59 points. The lowest and the highest quartile were analysed using binary logistic regression and presented as the odds ratio (OR) with 95% CI. The variables which exhibited statistical significance (p < 0.05) on univariate regression analysis were used in building the multivariable models.
Statistical analyses were performed employing the software SPSS Statistics for Windows (version 26), and a two-sided p-value threshold of < 0.05 was considered statistically significant.
Results
Out of 514 patients (mean age: 64.9 ±11.27 years; 41.1% female) enrolled in the study, 116 (22.6%) patients had CAD. The differences between patients with and without CAD in demographics, social characteristics, concomitant comorbidities, and therapy are shown in Supplementary Table SI. Patients with CAD were significantly older, more commonly male, with an elementary level of education, retired, former smokers, and more often had functional mobility with help compared to non-CAD controls (all p-values ≤ 0.014). Furthermore, patients with CAD had a significantly higher prevalence of hypertension, heart failure, type 2 diabetes mellitus, and hyperlipoproteinaemia compared to non-CAD patients, while the diagnosis of AF was significantly more common in non-CAD patients (all p ≤ 0.009).
Self-reported treatment burden
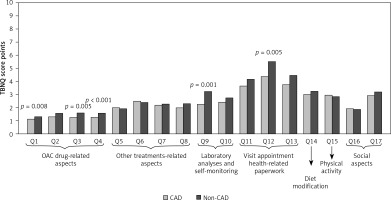
The mean self-reported TBN score was 40.49 ±21.54 points for patients with CAD and 46.17 ±21.44 points for patients without CAD, p = 0.023. There was no significant difference in the prevalence of TBN score of ≥ 59 points between the two groups (19.0% vs. 25.1%, respectively, p = 0.170). With respect to individual components of the TBN, patients with CAD reported significantly lower scores in relation to questions concerning laboratory tests, arranging appointments, and doctor visits, as well as the first, third, and fourth question about taking an oral anticoagulant (OAC) compared to non-CAD controls (all p-values ≤ 0.008); Figure 1.
Multivariable regression analysis
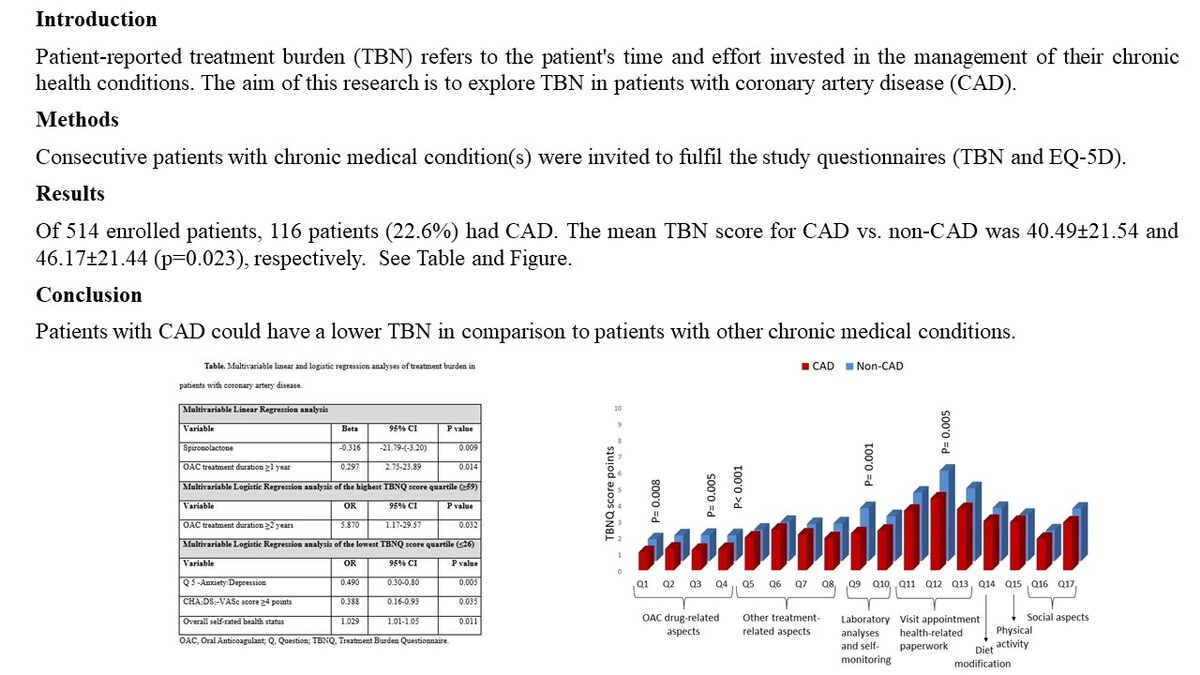
Univariate regression analysis within CAD and non-CAD groups is presented in Supplementary Tables SII and SIII. On multivariable analysis of the TBN questionnaire score as a continuous variable within the CAD group, the OAC treatment duration of ≥ 1 year was associated with an increased likelihood of having higher TBN (β = –0.316, 95% CI: –21.79-(–3.20), p = 0.009), while the use of spironolactone was associated with an increased likelihood of having lower TBN (β = 0.297, 95% CI: 2.75–23.89, p = 0.014); Table I. On multivariable analysis of the TBN score quartiles within the CAD group, OAC treatment duration ≥ 2 years was a significant predictor of the highest TBN score quartile (OR = 5.870, 95% CI: 1.17–29.57, p = 0.032).
Table I
Multivariable linear and logistic regression analyses of treatment burden in patients with coronary artery disease
The overall self-rated health status score was positively associated with the lowest TBN quartile (OR = 1.029, 95% CI: 1.01–1.05, p = 0.011), while question 5 (Q5) of the EQ-5D questionnaire regarding anxiety/depression and a CHA2DS2-VASc score of ≥ 4 points were inversely associated with the lowest TBN quartile (OR = 0.490, 95% CI: 0.30–0.80, p = 0.005 and OR = 0.388, 95% CI: 0.16–0.93, p = 0.035, respectively) within the CAD group.
Notably, the variables diabetes mellitus, insulin therapy, and number of parenteral applications daily, which demonstrated significance in univariate analysis, did not retain significance in the multivariable analysis. In comparison to CAD patients, multivariable factors were different among non-CAD patients, as presented in Supplementary Table SIV.
Discussion
To our knowledge, this is the first study to measure TBN in CAD patients. Our study shows the following: i) patients with CAD had a significantly lower TBN score in comparison to patients without CAD, ii) 1 in 5 CAD patients reported a TBN of ≥ 59 points, deemed to be unacceptably high from the patients’ perspective, and iii) using OAC for one year or longer was a positive predictor of higher TBN in patients with CAD, while an OAC treatment duration of 2 years or longer was a positive predictor of the highest TBN of ≥ 59 points.
In the present analysis, the mean TBN score in patients with CAD was 40 points, which is lower than the previously reported mean TBN score in patients with AF of 47 points [6]. Indeed, AF is a specific chronic disease which could burden patients with, for instance, frequent highly symptomatic episodes of AF that require doctor and/or hospital visits, changes in antiarrhythmic drug therapy, comprehensive concomitant risk factors and comorbidity management, and so forth. On the other hand, patients with CAD rarely have more than several episodes of acute coronary syndromes in their lifetime.
Regarding specific domains of the TBN questionnaire, the greatest contributors to the TBN score in patients with CAD were questions regarding doctor visits, administrative aspects, diet, and physical recommendations, which aligns with previous studies in patients with other chronic health conditions [6, 7, 9].
In the present analysis, 19% of patients with CAD reported unacceptably high TBN (≥ 59 points), in line with a large study from France of 2413 patients with various chronic medical conditions, which reported that a total of 28% of participants declared an unacceptably high TBN, ranging from 19% of patients with cardiac conditions to 50% of those with asthma [5].
In our study, patients with CAD reported significantly lower TBN in comparison to patients without CAD. However, patients with CAD reported a significantly lower quality of life and more commonly had multimorbidity and polypharmacy compared to those without CAD, which is apparently paradoxical. A possible explanation could be because patients without CAD had a significantly higher prevalence of AF and female sex. We found that in non-CAD patients atrial fibrillation was a multivariable predictor of higher TBN; see Supplementary Table SIV. Our previous research has indicated that patients with AF (especially females) have significantly higher TBN compared to those without AF [6, 7]. Furthermore, patients with CAD reported significantly lower scores for questions regarding laboratory analysis and other examinations, arranged appointments and scheduled doctor visits compared to patients without CAD. This finding could be explained by better coordination of diagnosis and treatment pathways for patients with CAD, including the establishment of ST-elevation myocardial infarction (STEMI) networks [10]. Furthermore, the initial manifestation of CAD is often characterised by specific symptoms in most patients, while in other cardiac diseases such as AF, the clinical presentation could be nonspecific, and a patient may undergo examinations by various specialities before being seen by a cardiologist for definitive diagnosis and treatment of AF, which could impose a significant burden on patients.
OAC use is associated with a higher bleeding risk and dietary modification, which could affect the patient’s TBN over time. As a consequence, and perhaps not unexpectedly, in multivariable regression analysis we found that longer use of OAC was an independent positive predictor of higher TBN and unacceptably high TBN in patients with CAD. Additionally, we found that the utilization of spironolactone therapy was an independent predictor of lower TBN, and a possible explanation is that spironolactone therapy is commonly employed in the management of heart failure, contributing to heart failure symptom regulation and potentially reducing the necessity for repeated medical consultations.
Limitations
This study was a pilot, cross-sectional, single-centre study with a relatively small cohort, which could have influenced the results. Additionally, we did not capture data regarding other factors that could have impacted the results, such as health literacy, cognitive function, etc. Given that the vast majority of citizens of Serbia have extensive public health insurance, we excluded the question regarding financial burden, which could have influenced the results of TBN in other countries.
In conclusion, this was the first study that specifically addressed TBN in patients with CAD. Our findings suggest that patients with CAD could have a lower TBN in comparison to patients with other chronic medical conditions, possibly owing to a better-structured diagnosis and management pathways pertinent to CAD. Nevertheless, 1 in 5 patients with CAD experienced an unacceptably high TBN, thus indicating that optimisation in the long-term management of patients with CAD is still needed. Further research is needed to comprehensively characterise the patient-reported TBN and its implications in patients with CAD.