Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
Editor's Choice
NUTRITION / CLINICAL RESEARCH
Assessing the impact of a wheat flour and baker’s yeast restricted diet vs. calorie restriction in non-alcoholic fatty liver disease patients
1
Department of Endocrinology and Metabolism, Sivas Numune Hospital, Sivas, Turkey
2
University of Montenegro-Faculty of Medicine, Podgorica, Montenegro
3
Center for Laboratory Diagnostics, Primary Health Care Center, Podgorica, Montenegro
4
Department of Endocrinology and Metabolism, Faculty of Medicine, Erzurum Regional Education and Research Hospital, Erzurum, Turkey
5
Department of Medical Biochemistry, University of Belgrade-Faculty of Pharmacy, Belgrade, Serbia
6
Department of Radiology, Faculty of Medicine, Giresun Regional Education and Research Hospital, Giresun, Turkey
7
Department of Endocrinology and Metabolism, Batman Training and Research Hospital, Batman, Turkey
8
Department of Endocrinology and Metabolism, Faculty of Medicine, Ataturk University, Erzurum, Turkey
9
Department of Endocrinology and Metabolism, Faculty of Medicine, Recep Tayyip Erdogan University, Rize, Turkey
Submission date: 2024-07-13
Final revision date: 2024-09-05
Acceptance date: 2024-09-14
Online publication date: 2024-10-26
Corresponding author
Filiz Mercantepe
Recep Tayyip Erdogan University, Recep Tayyip Erdogan Universirty, 53010, Rize, Turkey
Recep Tayyip Erdogan University, Recep Tayyip Erdogan Universirty, 53010, Rize, Turkey
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Non-alcoholic fatty liver disease (NAFLD) is a prevalent and nonalcoholic, progressive liver disorder associated with metabolic disturbance. This study aimed to compare the efficacy of a wheat flour or baker’s yeast restricted diet with traditional calorie restriction in NAFLD patients.
Material and methods:
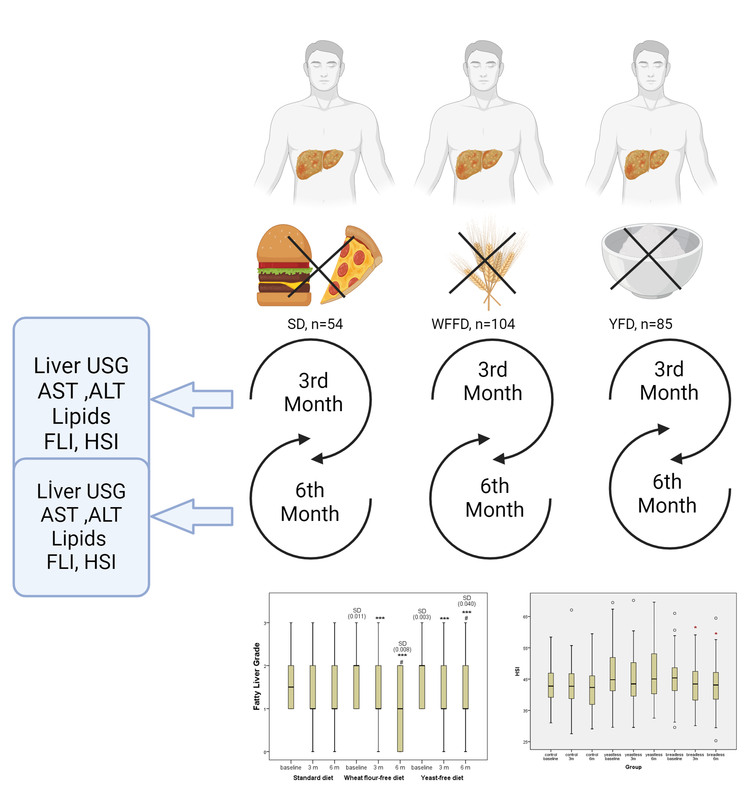
The analysed data were obtained from 243 individuals with NAFLD, who completed the study. Of these patients, 54 belonged to Group (1) (standard diet, SD), 104 belonged to Group (2) (wheat flour-free diet, WFFD), and 85 belonged to Group (3) (yeast-free diet, YFD). The intervention period lasted 6 months, during which participants’ dietary compliance was closely monitored. Anthropometric measurements, liver function tests, and imaging studies were conducted at baseline, after 3 months, and at the endpoint.
Results:
At the end of the 6-month trial, both the WFFD and HFD groups exhibited a noteworthy reduction in body mass index (BMI) and triglyceride (TG) levels when compared to a standard diet that only involved calorie restriction. Furthermore, a notable reduction in the severity of liver steatosis was seen in these groups (p < 0.05). The SD group did not exhibit any significant changes in these metrics. The WFFD group experienced a notable reduction in Hepatic Steatosis Index (HSI) values (p < 0.05). Cluster analysis revealed that the obese group had higher HSI, weight, and BMI values throughout the study period, indicating a more advanced stage of NAFLD.
Conclusions:
This study highlights the significance of food constituents and dietary strategies in the treatment of NAFLD. It suggests that limiting the intake of wheat flour and baker’s yeast specifically could have positive effects on liver well-being. Nevertheless, it is imperative to conduct comprehensive and enduring investigations that consider the genetic and metabolic variations among individuals. The results of this study provide evidence that customised dietary approaches designed to meet people’s specific nutritional requirements could be crucial in the treatment of NAFLD.
Non-alcoholic fatty liver disease (NAFLD) is a prevalent and nonalcoholic, progressive liver disorder associated with metabolic disturbance. This study aimed to compare the efficacy of a wheat flour or baker’s yeast restricted diet with traditional calorie restriction in NAFLD patients.
Material and methods:
The analysed data were obtained from 243 individuals with NAFLD, who completed the study. Of these patients, 54 belonged to Group (1) (standard diet, SD), 104 belonged to Group (2) (wheat flour-free diet, WFFD), and 85 belonged to Group (3) (yeast-free diet, YFD). The intervention period lasted 6 months, during which participants’ dietary compliance was closely monitored. Anthropometric measurements, liver function tests, and imaging studies were conducted at baseline, after 3 months, and at the endpoint.
Results:
At the end of the 6-month trial, both the WFFD and HFD groups exhibited a noteworthy reduction in body mass index (BMI) and triglyceride (TG) levels when compared to a standard diet that only involved calorie restriction. Furthermore, a notable reduction in the severity of liver steatosis was seen in these groups (p < 0.05). The SD group did not exhibit any significant changes in these metrics. The WFFD group experienced a notable reduction in Hepatic Steatosis Index (HSI) values (p < 0.05). Cluster analysis revealed that the obese group had higher HSI, weight, and BMI values throughout the study period, indicating a more advanced stage of NAFLD.
Conclusions:
This study highlights the significance of food constituents and dietary strategies in the treatment of NAFLD. It suggests that limiting the intake of wheat flour and baker’s yeast specifically could have positive effects on liver well-being. Nevertheless, it is imperative to conduct comprehensive and enduring investigations that consider the genetic and metabolic variations among individuals. The results of this study provide evidence that customised dietary approaches designed to meet people’s specific nutritional requirements could be crucial in the treatment of NAFLD.
REFERENCES (35)
1.
Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: from pathophysiology to therapeutics. Metabolism 2019; 92: 82-97.
2.
Mitrovic B, Gluvic ZM, Obradovic M, et al. Non-alcoholic fatty liver disease, metabolic syndrome, and type 2 diabetes mellitus: where do we stand today? Arch Med Sci 2023; 19: 884-94.
3.
Rinella ME, Lazarus JV, Ratziu V, et al.; NAFLD Nomenclature consensus group. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. Hepatology 2023; 78: 1966-86.
4.
Meneses D, Olveira A, Corripio R, et al. Performance of noninvasive liver fibrosis scores in the morbid obese patient, same scores but different thresholds. Obes Surg 2020; 30: 2538-46.
5.
Zhou XD, Targher G, Byrne CD, et al. An international multidisciplinary consensus statement on MAFLD and the risk of CVD. Hepatol Int 2023; 17: 773-91.
6.
Pan Q, Fan JG, Yilmaz Y. Pathogenetic pathways in nonalcoholic fatty liver disease: an incomplete Jigsaw puzzle. Clin Liver Dis 2023; 27: 317-32.
7.
Klisic A, Kavaric N, Abenavoli L, et al. Is endocan a novel potential biomarker of liver steatosis and fibrosis? J Med Biochem 2020; 39: 363-71.
8.
Rafaqat S, Gluscevic S, Mercantepe F, Rafaqat S, Klisic A. Interleukins: pathogenesis in non-alcoholic fatty liver disease. Metabolites 2024; 14: 153.
9.
Park J, Kim G, Kim H, et al. The association of hepatic steatosis and fibrosis with heart failure and mortality. Cardiovasc Diabetol 2021; 20: 197.
10.
Tian F, Guo Y, Zhou L, et al. Comparison of glimepiride and linagliptin in the treatment of non-alcoholic hepatic disease with type 2 diabetes mellitus. Arch Med Sci DOI: https://doi.org/10.5114/aoms/1....
11.
Brboric J, Klisic A, Kotur-Stevuljevic J, et al. Natural and natural-like polyphenol compounds: in vitro antioxidant activity and potential for therapeutic application. Arch Med Sci 2023; 19: 651-71.
12.
Perdomo CM, Frühbeck G, Escalada J. Impact of nutritional changes on nonalcoholic fatty liver disease. Nutrients 2019; 11: 677.
13.
Suárez M, Boqué N, del Bas JM, Mayneris-Perxachs J, Arola L, Caimari A. Mediterranean diet and multi-ingredient-based interventions for the management of non-alcoholic fatty liver disease. Nutrients 2017; 9: 1052.
14.
Anania C, Massimo Perla F, Olivero F, Pacifico L, Chiesa C. Mediterranean diet and nonalcoholic fatty liver disease. World J Gastroenterol 2018; 24: 2083-94.
15.
Watanabe M, Tozzi R, Risi R, et al. Beneficial effects of the ketogenic diet on nonalcoholic fatty liver disease: a comprehensive review of the literature. Obes Rev 2020; 21: e13024..
16.
Wang H, Wang L, Cheng Y, Xia Z, Liao Y, Cao J. Efficacy of orlistat in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Biomed Reports 2018; 9: 90-6.
17.
Riazi K, Raman M, Taylor L, Swain MG, Shaheen AA. Dietary patterns and components in nonalcoholic fatty liver disease (NAFLD): what key messages can health care providers offer? Nutrients 2019; 11: 2878.
18.
Aguiar EV, Santos FG, Krupa-Kozak U, Capriles VD. Nutritional facts regarding commercially available gluten-free bread worldwide: recent advances and future challenges. Crit Rev Food Sci Nutr 2023; 63: 693-705.
19.
Mohamed DA, Abdelgayed SS, Essa HA, Mohamed RS. Preparation and evaluation of functional foods for prevention of non-alcoholic fatty liver disease. Pakistan J Biol Sci 2018; 21: 454-62.
20.
Nehmi-Filho V, Santamarina AB, de Freitas JA, et al. Novel nutraceutical supplements with yeast -glucan, prebiotics, minerals, and Silybum marianum (silymarin) ameliorate obesity-related metabolic and clinical parameters: a double-blind randomized trial. Front Endocrinol (Lausanne) 2023; 13: 1089938.
21.
Liu Q, Liu S, Chen L, et al. Role and effective therapeutic target of gut microbiota in NAFLD/NASH (review). Exp Ther Med 2019; 18: 1935-44.
22.
Demir M, Lang S, Hartmann P, et al. The fecal mycobiome in non-alcoholic fatty liver disease. J Hepatol 2022; 76: 788-99.
23.
Xie C, Halegoua-Demarzio D. Role of probiotics in non-alcoholic fatty liver disease: does gut microbiota matter? Nutrients 2019; 11: 2837.
24.
Asgharpour A, Cazanave SC, Pacana T, et al. A diet-induced animal model of non-alcoholic fatty liver disease and hepatocellular cancer. J Hepatol 2016; 65: 579-88.
25.
Lee JH, Kim D, Kim HJ, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis 2010; 42: 503-8.
26.
De Lucia Rolfe E, Brage S, Sleigh A, et al. Validity of ultrasonography to assess hepatic steatosis compared to magnetic resonance spectroscopy as a criterion method in older adults. PLoS One 2018; 13: 87-99.
27.
Hackensack N. Handbook of medical statistics. 1st ed. Singapore: World Scientific Publishing Co. Pte. Ltd.; 2017.
29.
Katsiki N, Stoian Pantea A, Rizzo M. Dietary patterns in non-alcoholic fatty liver disease (NAFLD): stay on the straight and narrow path! Clín Investig En Arterioscler 2022; 34: 24-31.
30.
Kwanten WJ. Diet and non-alcoholic fatty liver disease, a short narrative review. Acta Gastroenterol Belg 2023; 86: 306-10.
31.
Ullah R, Rauf N, Nabi G, et al. Role of nutrition in the pathogenesis and prevention of non-alcoholic fatty liver disease: recent updates. Int J Biol Sci 2019; 15: 265-76.
32.
Quesada-Vázquez S, Aragonès G, Del Bas JM, Escoté X. Diet, gut microbiota and non-alcoholic fatty liver disease: three parts of the same axis. Cells 2020; 9: 176.
33.
Klisic A, Isakovic A, Kocic G, et al. Relationship between oxidative stress, inflammation and dyslipidemia with fatty liver index in patients with type 2 – diabetes mellitus. Exp Clin Endocrinol Diabetes 2018; 126: 371-8.
34.
Klisic A, Kavaric N, Jovanovic M, Soldatovic I, Gligorovic-Barhanovic N, Kotur-Stevuljevic J. Bioavailable testosterone is independently associated with Fatty Liver Index in postmenopausal women. Arch Med Sci 2017; 13: 1188-96.
35.
Della Torre S. Beyond the x factor: relevance of sex hormones in NAFLD pathophysiology. Cells 2021; 10: 2502.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.