Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors NEW
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
METABOLIC DISORDERS / EXPERIMENTAL RESEARCH
Aloperin improves liver non-alcoholic steatohepatitis
in vitro and in vivo
1
Department of Infection Diseases and Liver Diseases, The First Affiliated Hospital of Shandong First Medical University (Shandong Provincial Qianfoshan Hospital), Jinan, China
2
Department of Hepatology, Beijing Ditan Hospital Capital Medical University, Beijing, China
3
PCR laboratory,The First Affiliated Hospital of Shandong First Medical University (Shandong Provincial Qianfoshan Hospital), Jinan, China
4
Department of Clinical Pathology, The First Affiliated Hospital of Shandong First Medical University (Shandong Provincial Qianfoshan Hospital), Jinan, China
Submission date: 2020-01-06
Final revision date: 2020-01-31
Acceptance date: 2020-02-06
Online publication date: 2020-05-25
Publication date: 2025-02-28
Arch Med Sci 2025;21(1):285-297
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The aim of this work is to investigate the inhibitory effect of aloperin (Alo) on hepatocyte apoptosis in non-alcoholic fatty liver disease, and the underlying mechanism.
Material and methods:
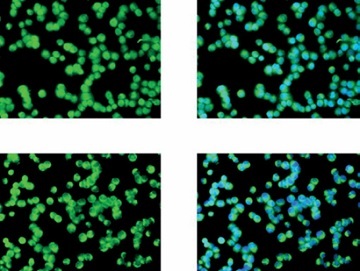
Rats in the Alo groups were fed a high-fat + high-sugar diet for 8 weeks and then treated with low-, moderate-, and high-dose Alo for another 8 weeks via gavage. Oxidative stress indices were tested by a colourimetric method, and pathological changes were observed by haematoxylin–eosin staining. Apoptosis was detected by TUNEL staining. TLR4, TRIF, and NF-κB(p65) mRNA and protein expressions were detected by RT-qPCR, Western blot assay and immunohistochemistry. In the in vitro study, L02 cells were treated with FFA (free fatty acid) for 24 h to establish a non-alcoholic steatohepatitis (NASH) model. Inhibition of cell proliferation was measured by the MTT method, and cell apoptosis was evaluated by flow cytometry. Finally, the nuclear import volume of NF-κB(p65) was evaluated by cellular immunofluorescence.
Results:
Cell apoptosis significantly decreased in the Alo-treatment groups in a dose-dependent manner (p < 0.05). TLR4, TRIF, and NF-κB(p65) expression in the Alo-treatment groups was significantly downregulated compared with model group (p < 0.05). The cell proliferation rate significantly increased, cell apoptosis significantly decreased (p < 0.05), and the TLR4/TRIF/NF-κB pathway was significantly inhibited (p < 0.05) in the Alo-treatment groups. The nuclear import volume of NF-κB(p65) in the Alo-treatment groups was significantly decreased compared with that in the model group in a dose-dependent manger (p < 0.05).
Conclusions:
Alo could improve NASH via the TLR4/TRIF/NF-κB pathway.
The aim of this work is to investigate the inhibitory effect of aloperin (Alo) on hepatocyte apoptosis in non-alcoholic fatty liver disease, and the underlying mechanism.
Material and methods:
Rats in the Alo groups were fed a high-fat + high-sugar diet for 8 weeks and then treated with low-, moderate-, and high-dose Alo for another 8 weeks via gavage. Oxidative stress indices were tested by a colourimetric method, and pathological changes were observed by haematoxylin–eosin staining. Apoptosis was detected by TUNEL staining. TLR4, TRIF, and NF-κB(p65) mRNA and protein expressions were detected by RT-qPCR, Western blot assay and immunohistochemistry. In the in vitro study, L02 cells were treated with FFA (free fatty acid) for 24 h to establish a non-alcoholic steatohepatitis (NASH) model. Inhibition of cell proliferation was measured by the MTT method, and cell apoptosis was evaluated by flow cytometry. Finally, the nuclear import volume of NF-κB(p65) was evaluated by cellular immunofluorescence.
Results:
Cell apoptosis significantly decreased in the Alo-treatment groups in a dose-dependent manner (p < 0.05). TLR4, TRIF, and NF-κB(p65) expression in the Alo-treatment groups was significantly downregulated compared with model group (p < 0.05). The cell proliferation rate significantly increased, cell apoptosis significantly decreased (p < 0.05), and the TLR4/TRIF/NF-κB pathway was significantly inhibited (p < 0.05) in the Alo-treatment groups. The nuclear import volume of NF-κB(p65) in the Alo-treatment groups was significantly decreased compared with that in the model group in a dose-dependent manger (p < 0.05).
Conclusions:
Alo could improve NASH via the TLR4/TRIF/NF-κB pathway.
REFERENCES (21)
1.
Carr RM, Oranu A, Khungar V. Nonalcoholic fatty liver disease-pathophysiology and management. Gastroenterol Clin North Am 2016; 45: 639-52.
2.
Beyaz MO, Ugurlucan M, Oztas DM, et al. Evaluation of the relationship between plaque formation leading to symptomatic carotid artery stenosis and cytomegalovirus by investigating the virus DNA. Arch Med Sci Atheroscler Dis 2019; 4: e19-24.
3.
Shen X, Guo H, Xu J, Wang J. Inhibition of lncRNA HULC improves hepatic fibrosis and hepatocyte apoptosis by inhibiting the MAPK signaling pathway in rats with nonalcoholic fatty liver disease. J Cell Physiol 2019; 234: 18169-79.
4.
Bassler J, Ducatman A, Elliott M, et al. Environmental perfluoroalkyl acid exposures are associated with liver disease characterized by apoptosis and altered serum adipocytokines. Environ Pollut 2019; 247: 1055-63.
5.
Guan CP, Luo HX, Fang HE, Zhou XZ. Global transcriptome changes of biofilm-forming staphylococcus epidermidis responding to total alkaloids of sophorea alopecuroides. Pol J Microbiol 2018; 67: 223-6.
6.
Sinphitukkul K, Manotham K, Eiam-Ong S, Eiam-Ong S. Aldosterone nongenomically induces angiotensin II receptor dimerization in rat kidney: role of mineralocorticoid receptor and NADPH oxidase. Arch Med Sci 2019; 15: 1589-98.
7.
Guo C, Yang L, Wan CX, et al. Anti-neuroinflammatory effect of Sophoraflavanone G from Sophora alopecuroides in LPS-activated BV2 microglia by MAPK, JAK/STAT and Nrf2/HO-1 signaling pathways. Phytomedicine 2016; 23: 1629-37.
8.
Tian A, Xu T, Liu K, Zou Q, Yan X. Anti-Helicobacter pylori effect of total alkaloids of sophora alopecuroides in vivo. Chin Med J (Engl) 2014; 127: 2484-91.
9.
Zhou Y, Wang H, Liang L, Zhao WC, Chen Y, Deng HZ. Total alkaloids of Sophora alopecuroides increases the expression of CD4+ CD25+ Tregs and IL-10 in rats with experimental colitis. Am J Chin Med 2010; 38: 265-77.
10.
Shen XD, Ke B, Zhai Y, et al. Toll-like receptor and heme oxygenase-1 signaling in hepatic ischemia/reperfusion injury. Am J Transplant 2005; 5: 1793-800.
11.
Zheng D, Li Z, Wei X, et al. Role of miR-148a in mitigating hepatic ischemia-reperfusion injury by repressing the TLR4 signaling pathway via targeting CaMKIIalphain vivo and in vitro. Cell Physiol Biochem 2018; 49: 2060-72.
12.
Nabih ES, El-Kharashi OA. Targeting HMGB1/TLR4 axis and miR-21 by rosuvastatin: role in alleviating cholestatic liver injury in a rat model of bile duct ligation. Naunyn Schmiedebergs Arch Pharmacol 2019; 392: 37-43.
13.
Wigg AJ, Roberts-Thomson IC, Dymock RB, McCarthy PJ, Grose RH, Cummins AG. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor alpha in the pathogenesis of non-alcoholic steatohepatitis. Gut 2001; 48: 206-11.
14.
Jokelainen K, Reinke LA, Nanji AA. NF-kappaB activation is associated with free radical generation and endotoxemia and precedes pathological liver injury in experimental alcoholic liver disease. Cytokine 2001; 16: 36-9.
15.
Chen Y, Ma K. NLRC4 inflammasome activation regulated by TNF-alpha promotes inflammatory responses in nonalcoholic fatty liver disease. Biochem Biophys Res Commun 2019; 511: 524-30.
16.
Wang C, Choi YH, Xian Z, Zheng M, Piao H, Yan G. Aloperine suppresses allergic airway inflammation through NF-kappaB, MAPK, and Nrf2/HO-1 signaling pathways in mice. Int Immunopharmacol 2018; 65: 571-9.
17.
Fu X, Sun F, Wang F, et al. Aloperine protects mice against DSS-induced colitis by PP2A-mediated PI3K/Akt/mTOR signaling suppression. Mediators Inflamm 2017; 2017: 5706152.
18.
Ren D, Ma W, Guo B, Wang S. Aloperine attenuates hydrogen peroxide-induced injury via anti-apoptotic activity and suppression of the nuclear factor-kappaB signaling pathway. Exp Ther Med 2017; 13: 315-20.
19.
Van Antwerp DJ, Martin SJ, Kafri T, Green DR, Verma IM. Suppression of TNF-alpha-induced apoptosis by NF-kappaB. Science 1996; 274: 787-9.
20.
Wang CY, Mayo MW, Korneluk RG, Goeddel DV, Baldwin AS Jr. NF-kappaB anti-apoptosis: induction of TRAFland TRAF2 and c-IAPI and c-lAP2 to suppress caspase-8 activation. Science 1998; 281: 1680-3.
21.
Chen C, Edelstein LC, Gélinas C. The Rel/NF-kappaB family directly activates expression of the apoptosis inhibitor Bcl-x(L). Mol Cell Biol 2000; 20: 2687-95.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.