Sjögren’s syndrome (SS) and rheumatoid arthritis (RA) are two types of chronic autoimmune diseases. Sjögren’s syndrome is characterised by lymphocytes infiltrating the exocrine glands, resulting in dry mouth and dry eyes [1]. Rheumatoid arthritis is a chronic, inflammatory, connective tissue disease, leading to foot deformities, impairment of locomotive functions and reductions in patients’ quality of life [2]. The two diseases may exist alone or overlap. In this case, the patient presented with acute renal failure caused by SS and RA overlap syndrome, which is rarely reported in the literature. Through a case analysis, this article discusses the association between the two diseases, the treatment options and prognosis after renal damage occurs and the relevant literature.
Methods
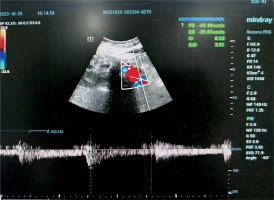
A 66-year-old female farmer was admitted to the hospital after experiencing nausea and vomiting for more than 20 days and elevated serum creatinine for 2 h. The patient’s previous history included RA for more than 30 years. Her physical examination on admission showed tooth loss, dry mouth, dry eyes and multiple skeletal joint deformities. The laboratory test from the Key Laboratory of Bone Metabolism and Physiology in Chronic Kidney Disease of Hebei Province, Test result showed the following: serum creatinine 255 µmol/l, bicarbonate 7 mmol/l, potassium 3.2 mmol/l, urine occult blood 2+, urine protein 1+, urine glucose 1+, urine albumin-to-creatinine ratio 236 mg/g, urine protein/creatinine 1,902.83 mg/g and negative antineutrophil cytoplasmic antibodies. The urinary ultrasound showed diffuse lesions in both kidneys (Figure 1). The immunological indicators were as follows: rheumatoid factor 807 IU/l (normal range: 0–20 IU/l), immunoglobulin G (IgG) 12.20 g/l (normal range: 7.0–16.6 g/l), IgG4 5.1 g/l (normal range: 0.6–1.1 g/l), immunoglobulin A 8.83 g/l (normal range: 0.76–3.9 g/l), immunoglobulin M 4.54 g/l (normal range: 0.35–5.5 g/l) and complement C3 0.46 g/l (normal range: 0.85–1.7 g/l); antinuclear antibody positive, antinuclear granule type 1:320 and nucleolar type 1:320; and anti-SSA antibody, anti-SSB antibody and anti-Ro-52 antibody were positive. The patient’s thyroid function was normal: thyroid stimulating hormone 2.9 mIU/l (normal 0.4–4.0 mIU/l), free triiodothyronine (FT) 3 3.4 pmol/l (normal 3.1–6.8 pmol/l) and FT4 17.1 pmol/l (normal 12.0–22.0 pmol/l). Her anti-thyroid peroxidase antibody was 17 IU/ml (normal < 34 IU/ml), and her anti-thyroglobulin antibody was 19 IU/ml (normal < 115 IU/ml). The thyroid colour Doppler ultrasound demonstrated a hypoechoic nodule of the left thyroid lobe: Thyroid Imaging Reporting and Data System class 4a. The abdominal examination showed the following: blood lipase 3,991 U/l, blood amylase 480 U/l and albumin 31 g/l. Abdominal magnetic resonance imaging and enhanced scans were performed and detected a blood-rich nodule (about 1.5 × 1.4 cm) in front of the pancreatic head and neck junction.
Due to these results, acute renal failure caused by SS and RA overlap syndrome was considered clinically. Due to the patient’s bone and joint deformities, a renal biopsy was difficult to obtain; therefore, renal pathological data were not obtained. The patient was given a fluid infusion, nutritional support, 40 mg of methylprednisolone once a day, 0.2 g of hydroxychloroquine sulphate twice a day, a potassium citrate supplement and sodium bicarbonate correction. After 14 days of treatment, the patient’s nausea and vomiting were relieved. The patient’s serum creatinine was 103 µmol/l, bicarbonate was 17 mmol/l, potassium was 4.2 mmol/l, IgG4 was 4.5 g/l, lipase was 277.68 U/l and blood amylase was 197 U/l. The patient was then discharged from the hospital. After discharge, the patient continued to take two oral medications: 20 mg of methylprednisolone once a day and 0.2 g of hydroxychloroquine sulphate twice a day. The patient’s renal function, immunological indicators, pancreatic enzymes and thyroid function were regularly reviewed. After 6 months of follow-up, the patient’s general condition was good; she reported no nausea, vomiting, dry mouth, dry eyes or other discomfort, normal joint activity and no oedema. Upon re-examination the patient’s results were as follows: serum creatinine 88 µmol/l, bicarbonate 22 mmol/l, potassium 4.5 mmol/l, IgG4 3.8 g/l, lipase 198.76 U/l, blood amylase 176 U/l, thyroid function was normal and the size of the hypoechoic nodules in the left thyroid lobe demonstrated no significant changes. The size of the nodules with rich blood supply in the front of the pancreatic head and neck junction had decreased slightly, and the patient’s prognosis was favourable.
Discussion
The patient presented with haematuria, proteinuria, hypoalbuminaemia, elevated serum creatinine, renal tubular acidosis, hypokalaemia, dry mouth, dry eyes, joint deformity, a pancreatic mass, elevated pancreatic enzymes and a thyroid mass outside the kidney. The patient’s symptoms were significantly improved, and her serum creatinine decreased to 103 µmol/l after short-term symptomatic treatments (i.e. kidney-preserving and fluid-replacement therapies). According to the diagnostic criteria of the Chinese Medical Association Rheumatology Society [3], the patient was clinically diagnosed with SS and RA combined with clinical manifestations of renal damage revealed by laboratory examination results that demonstrated renal tubulointerstitial injury. Renal damage caused by SS and RA overlap syndrome should be considered in these patients; renal lesions involving the glomerulus, renal interstitium and renal tubules are uncommon in clinical work but are worthy of attention and consideration.
The patient had a long history of RA and came to our hospital with the primary complaint of acute renal failure. A review of relevant literature revealed that renal damage caused by rheumatoid vasculitis may clinically manifest as acute renal failure [4] and that haematuria and proteinuria are common. Additionally, perinuclear antineutrophil cytoplasmic antibody (ANCA) (myeloperoxidase-ANCA) can be positive in serum, but the serum ANCA test of this patient was negative. At the same time, the patient’s immunological examination showed that ANCA was positive: antinuclear granular type 1:320; nucleolar type 1:320; and anti-SSA antibody, anti-SSB antibody and anti-Ro-52 antibody were positive. With these results, SS was clinically confirmed, and the treating physician diagnosed the patient with acute renal failure caused by SS and RA overlap syndrome.
It has been reported that SS is present in up to 30% of patients with RA. Another study showed that 67.6% of patients with RA with both anti-SSA and anti-SSB antibodies were diagnosed with SS [5]. This patient had a 30-year history of an RA diagnosis accompanied by multiple skeletal joint deformities throughout the body (Figure 2). In addition, laboratory tests confirmed that the patient was positive for both anti-SSA and anti-SSB antibodies (Table I). The patient’s renal damage, therefore, may have resulted from the overlap of the two diseases.
Table I
Clinical examination results
Immunoglobulin G4-related disease (IgG4-RD) can invade any organ of the human body, and the pathogenesis is complex and changeable. Diagnoses may include pseudotumor, obliterative phlebitis and organ enlargement of the pancreas, kidney, lung, lacrimal gland or salivary gland [6]. In recent years, IgG4-RD has gained recognition in the medical community.
In the case presented in this article, the serum IgG4 level was increased and was accompanied by renal damage, class 4a thyroid nodules and rich blood supply nodules in the head and neck junction of the pancreas with significant increases in lipase and amylase. Therefore, IgG4-RD could not be excluded.
An elevated serum IgG4 level is often used as one of the diagnostic criteria for IgG4-RD both in China and globally, and a serum IgG4 ≥ 1.35 g/l is the recommended cut-off value for the diagnosis of IgG4-RD [7]. The serum IgG4 level was used to screen, evaluate and diagnose the patient presented in this article with IgG4-RD. In-depth studies of IgG4-RD have revealed that IgG4 is a unique antibody, and ongoing research is needed to further clarify its role. The imbalance of immune status and antibody synthesis caused by antigen exposure can trigger immune system diseases [8] characterised by a significant increase in the serum IgG4 level and the infiltration of IgG4-positive plasma cells in diseased tissues. Some studies have confirmed that serum IgG4 levels are elevated in patients with RA and that they may be a unique clinical manifestation of RA, closely related to disease activity and high levels of autoantibodies. They may also be a risk factor for RA [9] in patients with musculoskeletal system involvement, closely related [10] to disease activity and comorbidities. Additionally, it is generally believed that IgG4-RD is sensitive to glucocorticoids; as the treatment of the patient discussed in this case report demonstrates, the strategy is the same in patients with SS and RA overlap syndrome.
In conclusion, acute kidney injury caused by SS and RA overlap syndrome is relatively rare. This article presented a case report of a patient diagnosed with SS and RA overlap syndrome with elevated serum IgG4 levels. However, there are still a series of problems to be solved: (1) Renal impairment in RA is rare but it may be accompanied by elevated serum IgG4 levels. (2) The prognosis of renal function impairment in SS is good, but it is unclear whether the prognosis will be affected by RA. (3) This patient had blood-rich nodules in the pancreatic head and neck junction with significantly elevated lipase and amylase along with thyroid class 4a nodules. However, it has not yet been confirmed whether the IgG4 level has a pathogenic role in the disease. Similar cases must be evaluated to reveal the answers to these questions.