Introduction
Non-melanoma skin cancer encompasses a range of skin tumors, with the most prevalent being basal cell carcinoma and squamous cell carcinoma. Squamous cell carcinoma is a malignant tumor derived from keratinocytes in the epidermis, typically presenting as rough keratinizing papules, verrucous hyperplasia, or rapidly growing tender protrusions, often containing a central keratinous core. This condition poses a significant threat to the health and quality of life of affected individuals [1]. The main risk factors for cutaneous squamous cell carcinoma include exposure to ultraviolet radiation, ionizing radiation, HPV virus, chemical agents, immunosuppression, and chronic skin injury or inflammation [2]. In the United States alone, over 1 million cases of squamous cell carcinoma are diagnosed annually [3]. Moreover, studies have consistently demonstrated a global increase in the incidence of non-melanoma skin cancer [4, 5]. The substantial prevalence and large number of affected individuals undoubtedly contribute to a significant burden of disease, imposing substantial economic losses and placing immense pressure on healthcare systems. Consequently, it is important to analyze the global burden of non-melanoma skin cancer and develop appropriate strategies for public health prevention and control.
The Global Burden of Disease Study 2019 (GBD 2019), coordinated by the Institute for Health Metrics and Evaluation (IHME), estimated the burden of diseases, injuries, and risk factors for 204 countries and territories and selected subnational locations. The primary objective of this database is to quantify the global burden of various diseases on human health by utilizing disease burden indicators. Numerous studies have been conducted based on this database, offering a more comprehensive perspective on the global health status of different diseases.
Limited research has been conducted on the global disease burden of non-melanoma skin cancer. In this study, we examined the data on non-melanoma skin cancer from the GBD 2019 database, which provides information from 1990 to 2019. Indicators such as incident cases, incidence rate, disability-adjusted life years (DALYs), and DALY rate were used to assess the risk associated with this disease. We evaluated the disease burden and its changing patterns in various subgroups, including regions, countries, and age groups. Analyzing the GBD 2019 data can provide insights into the global burden of non-melanoma skin cancer and its temporal trends. This information can contribute to the development of effective health policies and prevention strategies aimed at reducing the burden of this disease.
Material and methods
Data sources
GBD 2019 data comes from Global Health Data Exchange GHDx) GHDx serves as a catalog of health-related data from around the world, covering various domains such as disease burden, risk factor analysis, age and sex stratification information, geographical distribution, and temporal trends, among others. The objective of this study is to quantitatively assess the global impacts of various diseases, injuries, and health risk factors on human health. Numerous investigations [6, 7] have extensively cited the burden of disease data contained within the GBD 2019 database, facilitating a systematic assessment of the worldwide distribution and trends in disease burden. These findings not only serve as a reliable foundation for global health research but also aid in policy development. This study is based on a publicly available database and does not require ethical approval.
Diagnostic criteria for diseases
Non-melanoma skin cancer is a malignancy that originates from squamous cells in the epithelium of the skin. Typically, it presents as a mass or ulcer on the skin, characterized by irregular margins and changes in color. The diagnosis is established through a pathologic examination of the tissue from the lesion. In the International Classification of Diseases (ICD-10), non-melanoma skin cancer is assigned the codes C44-C44.9, D04-D04.9, and D49.2. In the previous version, the ICD-9, the codes were 173-173.9, 222.4, 232-232.9, and 238.2.
Burden of disease data
The GBD 2019 database encompassed disease burden data from 204 countries and 21 world regions. In 2019, these countries were categorized into five groups based on their socio-demographic index (SDI): high SDI, high-middle SDI, middle SDI, low-middle SDI, and low SDI. SDI serves as a measure of overall socio-economic development and comprises three indicators: per capita income, average years of education, and fertility rate of the population under 25 years old. The index value ranges from 0 to 1, with higher values indicating greater levels of socio-economic and demographic advancement.
A range of disease burden indicators from the GBD 2019 database were chosen for analysis. These indicators include: incident cases, incidence rate, DALYs, and DALY rate.
Incident cases pertain to all individuals who show the first manifestation of a disease within a designated timeframe. This encompasses instances where individuals had not previously experienced the aforementioned condition, but have now exhibited symptoms for the first time during the period of inquiry. For each person being examined, only data from their first medical examination will be used. The incidence rate denotes the proportion of newly incurred cases in relation to either the overall population or the duration of exposure of a specific populace within a specified time frame. Typically, this rate is expressed in units of 1000 or 100,000 individuals.
DALYs represent a combined measure of years of life lost (YLL) and years lived with disability (YLD). This metric offers a comprehensive assessment of the impact that diseases have on both the duration and quality of individuals’ lives. To calculate DALYs, the following formula is employed: DALYs = YLL + YLD.
The DALY rate is used to standardize the total number of DALYs in a specific population. This metric offers a relative measure of how a disease impacts the overall health of a population, regardless of its size.
The age-standardized rate (ASR) is a useful tool for standardizing the measurement of disease burden, typically expressed per 100,000 individuals. It enables comparisons of disease measures across areas with varying population structures or within the same area over different time periods. The calculation of ASR is as follows:
Where ai denotes the index of disease burden in the ith age group, and wi denotes the corresponding standard population weight.
The estimated annual percentage change (EAPC) is a statistical indicator commonly employed in the domains of epidemiology and health research to depict time trends. The EAPC is determined by fitting the natural logarithm of age-standardized rates to best represent the change trend. The calculation of EAPC is done through the following formula: y = α + β x + ε, y = ln (γ), EAPC = 100 × (exp (β) – 1), where x represents the year, γ represents the standardized rate, and ε represents the residual. An EAPC greater than 0 indicates an upward trend in the index. The magnitude of the absolute value of EAPC corresponds to the significance of the upward trend. Conversely, an EAPC less than 0 indicates a downward trend in the indicators, with the magnitude of the absolute value of EAPC reflecting the significance of the downward trend. An EAPC equal to 0 signifies that the indicator remained relatively unchanged during the observation period.
Results
Trends in disease burden of non-melanoma skin cancer in different regions of the world from 1990 to 2019
Overall, these results suggest that from 1990 to 2019, there was an increase in the global age-standardized incidence rate (ASIR) for non-melanoma skin cancer, rising from 22.27 in 1990 to 30.30 in 2019. However, the age-standardized DALY rate remained relatively stable over the same time period. This indicates that while the incidence of non-melanoma skin cancer has been increasing globally, the overall burden of disease, as measured by DALYs, has not changed significantly. The EAPC for ASIR was 1.13 (95% CI: 0.50–1.77), highlighting a consistent upward trend. In contrast, the EAPC for the age-standardized DALY rate was 0.20 (95% CI: 0.10–0.30), demonstrating a much slower rate of change (Table I).
Table I
ASIR, age-standardized DALY rates and trends of non-melanoma skin cancer in regions of the world from 1990 to 2019
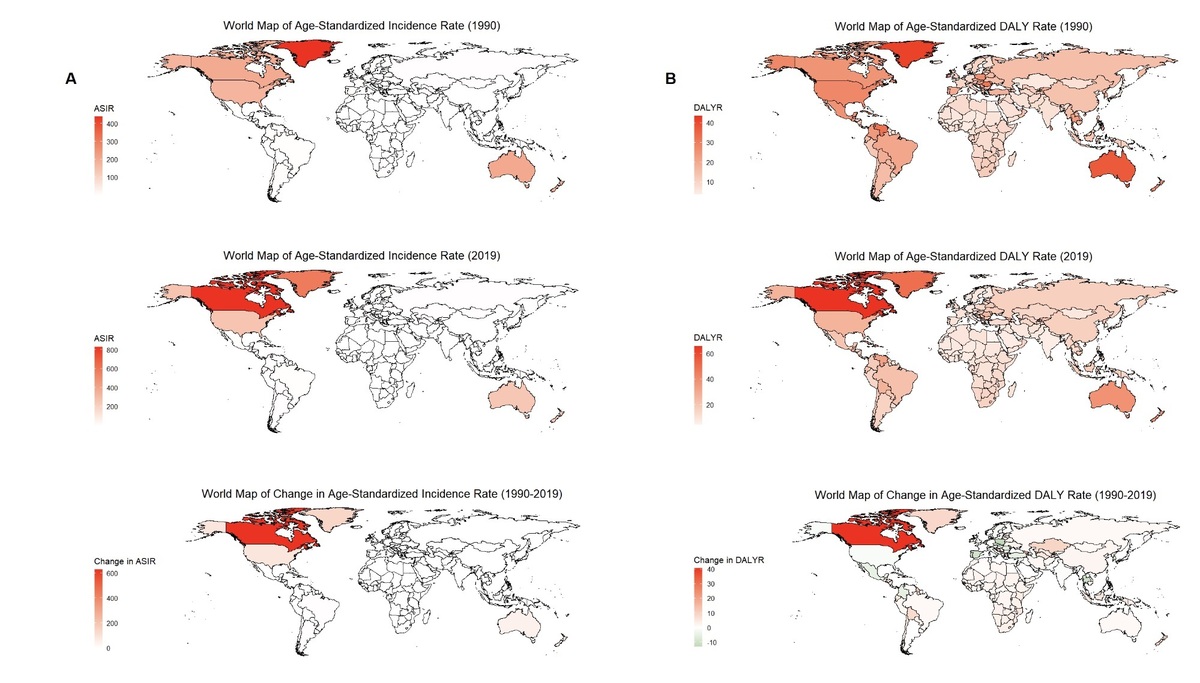
Among the 21 geographic regions in the GBD 2019 database, the ASIR for Australasia increased from 202.89 (95% uncertainty interval [8]: 174.68–233.86) in 1990 to 249.75 (95% UI: 210.03-294.74) in a region characterized by a heavy disease burden. In high-income North America, the ASIR increased from 179.63 (95% UI: 141.66–224.05) in 1990 to 324.18 (95% UI: 285.94–368.52), with an EAPC of 2.20 (95% confidence interval [CI]: 1.46–2.95), indicating a significant upward trend in disease burden. The age-standardized DALY rate for all geographic regions remained relatively stable from 1990 to 2019. Central Asia had the highest EAPC at 2.32 (95% CI: 2.05–2.60), while Central Europe had a negative EAPC of –1.35 (95% CI: –1.50, –1.20), demonstrating a declining trend in disease burden (Table I, Supplementary Table SI, Supplementary Figure S1).
Distribution of disease burden of non-melanoma skin cancer in different SDI regions of the world from 1990 to 2019
Countries with high SDI levels experienced higher incident cases and DALYs compared to countries with low SDI levels. From 1990 to 2019, the incident cases and DALYs of non-melanoma skin cancer showed a proportional increase across different SDI countries. No significant changes were observed in ASIR and age-standardized DALY rates in these countries. However, among the countries categorized based on SDI, those with high SDI had the highest ASIR, and its growth trend was the most significant (EAPC = 1.97, 95% confidence interval (CI): 1.30–2.65). On the other hand, high-middle SDI countries exhibited a downward trend in age-standardized DALY rates with an EAPC value of –0.36 (95% CI: –0.44, –0.27) (Table II, Supplementary Table SII, Supplementary Figure S2).
Table II
ASIR, age-standardized DALY rate and trends of non-melanoma skin cancer in countries of the world with different SDI levels from 1990 to 2019
Distribution of disease burden of non-melanoma skin cancer in different countries of the world from 1990 to 2019
In 2019, the United States of America (262.25), Greenland (576.15), and Canada (828.11) ranked as the top three countries with the highest ASIR. Conversely, Nepal (0.34), Bhutan (0.35), and Bangladesh (0.37) had the lowest ASIR. Regarding age-standardized DALY rates, Tonga (43.01), Greenland (49.97), and Canada (65.72) demonstrated the highest rates, while Egypt (4.48), Singapore (4.96), and the Syrian Arab Republic (5.28) exhibited the lowest rates. Between 1990 and 2019, the countries showing the most significant increases in ASIR were Canada (626.85), Greenland (137.07), and the United States of America (85.08). Likewise, Canada (40.51), Saint Kitts and Nevis (23.24), and Saint Vincent and the Grenadines (16.26) experienced the most substantial increases in age-standardized DALY rate (Supplementary Table SIII, Supplementary Figure S3).
The countries with high incident cases included the United States of America, Canada, and Australia, among others, while the countries with high DALYs were China, the United States of America, India, and others. Both the incident cases and DALYs exhibited a noticeable upward trend in countries worldwide from 1990 to 2019. Notably, countries such as the United Arab Emirates (10.67), Qatar (10.63), and Canada (9.07) experienced a higher proportion of incident cases. Likewise, the countries with the greatest proportion of DALYs increase were the United Arab Emirates (11.1), Saint Kitts and Nevis (10.12), and Qatar (8.19) (Supplementary Table SIV; Supplementary Figure S4).
The EAPC for cases, DALYs, and ASIR in each country were all greater than 0, demonstrating an overall increasing trend. Among them, Qatar (EAPC = 9.20, 95% CI: 8.74–9.67), United Arab Emirates (EAPC = 8.55, 95% CI: 8.16–8.95), and Canada (EAPC = 7.65, 95% CI: 7.46–7.84) showed the most significant increase in incident cases. The United Arab Emirates (EAPC = 9.12, 95% CI: 8.69–9.55), Qatar (EAPC = 8.19, 95% CI: 7.75–8.64), and Saint Kitts and Nevis (EAPC = 8.16, 95% CI: 6.76–9.58) exhibited the highest increase in DALYs. Canada (EAPC = 4.77, 95% CI: 4.60–4.93), Portugal (EAPC = 3.45, 95% CI: 3.15–3.75), and China (EAPC = 3.25, 95% CI: 3.07–3.43) showed the most obvious upward trend in ASIR. The change in the age-standardized DALY rate varied among countries, with Bosnia and Herzegovina (EAPC = 7.04, 95% CI: 6.20–7.89), Georgia (EAPC = 6.40, 95% CI: 5.53–7.27), and Saint Kitts and Nevis (EAPC = 6.02, 95% CI: 4.50–7.57) experiencing the greatest increase. Conversely, the Republic of Korea (EAPC = –4.03, 95% CI: –4.37, –3.69) and Poland (EAPC = –3.17, 95% CI: –3.62, –2.72) exhibited a downward trend in age-standardized DALY rate from 1990 to 2019 (Supplementary Table SIII; Supplementary Figure S5).
Comparison of disease burden of non-melanoma skin cancer between different genders in different regions of the world from 1990 to 2019
From 1990 to 2019, there was a consistent upward trend in the ASIR of non-melanoma skin cancer among both men and women in all countries across the globe. This trend was supported by the fact that the EAPC value exceeded 0. Additionally, the age-standardized DALY rate exhibited an increasing pattern in Asia, Africa, and North America.
The disease burden of non-melanoma skin cancer was more severe in males compared to females. In 1990 and 2019, Australasia and Southern Latin America had an ASIR of less than 1. Additionally, the ASIR of women in these regions was higher than that of men (Supplementary Table SV; Supplementary Figure S6).
Age distribution of non-melanoma skin cancer in different countries of the world in 2019
The incidence rate and DALYs of non-melanoma skin cancer among individuals aged 20 years and above in various countries worldwide in 2019 are depicted in the figure and table. In individuals aged 20–49 years, the incidence rate of non-melanoma skin cancer was notably low and did not exhibit a substantial increasing trend. Additionally, DALYs were lower in individuals aged 20-39 years. Conversely, for individuals aged 40 and above, both the incidence rate and DALYs of non-melanoma skin cancer displayed a significant increase with age. Furthermore, the disease burden associated with non-melanoma skin cancer was particularly severe among individuals aged over 80 years, as evidenced by the incidence rate and DALYs, which accounted for nearly half of the total population (Supplementary Tables SVI; SVII; Supplementary Figure S7).
Discussion
This study utilized the GBD 2019 database to classify global non-melanoma skin cancer into various subgroups, including region, SDI, country, gender, and age. A comprehensive data analysis was performed, examining incident cases, incidence rate, DALYs, DALY rate, age-standardized indicators, and EAPC.
The study results reveal variations in the disease burden of non-melanoma skin cancer across different regions and countries. Skin type strongly correlates with non-melanoma skin cancer, particularly in individuals with lighter skin, making it the most common malignancy. Moreover, the research indicates that residents in sunny regions and countries face a significantly elevated risk of developing non-melanoma skin cancer, owing to the close link between ultraviolet radiation and its incidence and mortality. These findings suggest that lower latitude regions may bear a more severe disease burden. The global disease burden of non-melanoma skin cancer exhibits regional disparities and geographic specialization. Consequently, there is a need to develop tailored control policies based on the distribution of this disease burden across different regions, with a particular focus on high-risk areas [8–10].
The disease burden of non-melanoma skin cancer was found to vary across different SDI regions. Previous studies have also linked this burden to social indicators, work environment, occupational class, and education level [11]. Individuals with higher socioeconomic status (SES) are at a higher risk of non-melanoma skin cancer, a finding consistent with our present study. This association may be attributed to the greater frequency of outdoor activities among individuals with high SES, leading to increased exposure to UV radiation, a known risk factor for non-melanoma skin cancer. Additionally, higher levels of awareness of non-melanoma skin cancer in rich people could lead to enhanced screening efforts. This, in turn, may result in more thorough documentation and reporting of cases.
Gender differences in the burden of disease are well documented [12–14], including in non-melanoma skin cancer. Globally, men have higher incidence and mortality rates for cancer compared to women [15, 16]. Specifically, the incidence of non-melanoma skin cancer is significantly higher in men than in women [17–19], with men experiencing three times higher incidence rates than women [20]. Aggarwal et al. [21], using relevant data, further found that non-melanoma skin cancer is twice as likely to cause death in men than in women. These disparities may be attributed to differences in occupational and lifestyle factors between genders. Men are more commonly exposed to UV light due to outdoor work, and evidence consistently links occupational UV exposure to non-melanoma skin cancer risk [22]. Moreover, men tend to use UV protective equipment less frequently than women, resulting in higher UV radiation exposure and increased disease risk.
Other studies have demonstrated a higher disease burden of non-melanoma skin cancer among the elderly, particularly evident in the increased incidence in individuals over 80 years old [23, 24]. Furthermore, the risk of non-melanoma skin cancer is higher in individuals aged 70 years and older across all age groups, while the incidence decreases significantly in those under 40 years old [25]. These observations may be attributed to the inevitable aging process of the skin with prolonged exposure to the natural environment, rendering skin cells more susceptible to carcinogenesis. The elderly typically have a weaker immune system, resulting in reduced clearance of abnormal cells and potentially increasing the risk of malignancies. Moreover, the evolving societal landscape has led to more diverse lifestyles, including an increase in outdoor activities, exposing individuals to higher levels of external ultraviolet radiation, a known carcinogen. Early diagnosis of diseases, such as cardiovascular disease and cancer, can be achieved through screening, leading to improved patient prognosis. Clinical diagnosis of non-melanoma skin cancer is challenging and susceptible to errors and misdiagnosis. Diagnosis typically involves dermoscopy and/or confocal microscopy, considering factors such as age, skin phototypes, previous diagnoses, sun exposure, and immunosuppression, alongside a thorough physical examination. It is essential to promote skin tumor screening norms to enhance public awareness, and for clinicians to actively identify skin cancer risk factors in their patients through routine skin examinations. Early detection allows for non-surgical treatments such as topical creams or photodynamic therapy, resulting in better long-term cosmetic outcomes, improved quality of life, and reduced morbidity and mortality associated with non-melanoma skin cancer.
However, it is important to acknowledge the limitations of this study. One limitation is that this analysis lacks consideration of the impact of the pandemic period 2020–2022, during which delays in diagnosis and access to effective treatment may have occurred due to limited access and fear of hospitalization. Moreover, there is potential variation in burden of disease data at the country level, which can be influenced by factors such as the size of the land area. For instance, countries with large land areas may experience significant differences in burden of disease between different regions, leading to inconsistencies across the entire country. Finally, the accuracy of burden of disease analysis is contingent upon the availability and quality of health data. Some regions may lack sufficient and reliable health data, which can result in inaccuracies when estimating the burden of disease for specific areas or populations. Furthermore, there may be delays in the collection and compilation of data related to disease burden, which can lead to inaccurate assessments of the current health status. Despite these limitations, it is essential to comprehensively understand the burden of disease to formulate effective prevention and control policies.
In conclusion, with the escalating disease burden of non-melanoma skin cancer globally, it is imperative to emphasize this matter, carry out extensive investigations, and evaluate its impact in order to provide scientific substantiation for the formulation of more efficacious intervention methodologies. Additionally, the influence of diverse factors on the disease burden of non-melanoma skin cancer necessitates further scrutiny and analysis, encompassing socio-cultural, economic, geographic, educational, and healthcare resource aspects. A more profound comprehension of the interplay among these factors can facilitate a more precise assessment and interpretation of the development and fluctuations in the disease burden of non-melanoma skin cancer.