Staphylococcus aureus (SA) is one of the most common pathogenic bacteria in bloodstream infection, accounting for 20% to 25% of all bloodstream infections and the 30-day mortality rate close to 20% [1, 2]. SA carries a variety of drug resistance genes and virulence genes, which are resistant to multiple antibiotics and its resistance could be transmitted among different strains, after acquiring resistance to methicillin [3]. The methicillin-resistant SA (MRSA) could induce a high incidence of mortality, which is an important risk factor for the death of patients with bloodstream infection [4].
Many studies have demonstrated the pleiotropic effects of statins including antibacterial activity, other than lowering cholesterol [5]. Some research studies on the antibacterial activity of statins, especially in the mechanism for changing the resistance of MRSA, achieved some positive results [6, 7]. Although many clinical research studies have confirmed its potential value in reducing patient mortality [8, 9], some studies did not find any benefit in reducing mortality or even showed harmful effects [10, 11]. This study retrospectively analyzed the effect of statins on drug resistance and mortality in patients with SA bloodstream infection.
Methods
Study design and population
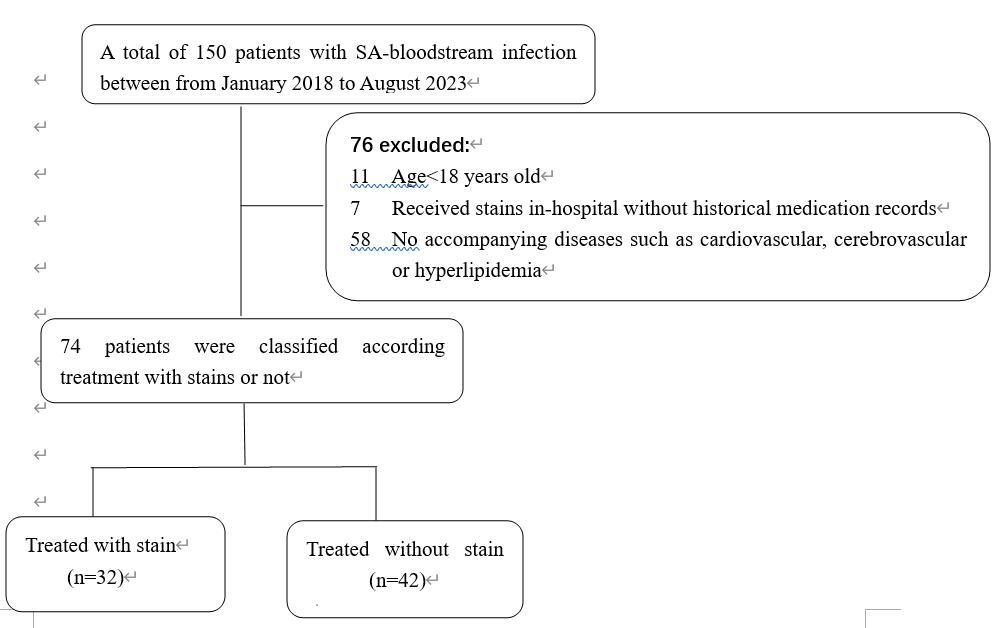
This is a retrospective single-center study, in which the electronic medical records of inpatients with SA bloodstream infection reported for the first time were analyzed from January 2018 to August 2023 in Dongguan Tungwah Hospital. The diagnosis of bloodstream infection meets the criteria of the U.S. Centers for Disease Control and Prevention including: SA was isolated from patients with one or more blood cultures; the patient has other clinical evidence of infection, at least one of the following symptoms or signs: fever (> 38°C), chills, or hypotension [12]. Age has a significant impact on different groups, as the teenager population (< 18 years) has fewer occurrences suffering from hypertension, hyperlipidemia, and other conditions that require statin treatment. Patients suffering only from chronic diseases with potential use of statins such as cardiovascular disease, cerebrovascular disease, or hyperlipidemia were included. Whether statins are finally used or not was decided by the attending physician. For patients receiving statins therapy, they must have received the same type of statin medicine before admission, and the treatment has not been interrupted throughout the entire hospitalization period. According to whether they received statins or not, the enrolled patients were divided into the statins group and non-statins group.
Microbiologic tests
All blood samples were sent to the microbiology laboratory of our hospital for culture, strain identification and in vitro drug sensitivity test. According to the Clinical and Laboratory Standards Institute (CLSI) standard interpretation of drug susceptibility test results, oxacillin resistance (MIC > 2 mg/l) was determined as MRSA [13].
Research outcomes
The primary end point was 30-day attributable mortality, and the difference of antimicrobial resistance between the two groups was the secondary end point. The risk factors for death due to SA bloodstream infection were further explored.
Statistical analysis
SPSS 22 software was used for statistical analysis of the data. Counting data were expressed as percentage and analyzed through χ2 test. Continuous data conforming to normal distribution were expressed as mean ± standard deviation and compared by independent sample t test. The comparison of abnormal distribution data adopts Wilcoxon non-parametric test.
Results
A total of 74 patients with SA bloodstream infection and underlying restricted diseases were included in the final analysis from January 2018 to August 2023 (Figure 1). There were 32 (43.2%) patients in the statins group and 42 (56.8%) patients in the non-statins group (Table I). Patients were predominantly male in both groups (non-statins group 64.3%, statins group 75.0%) and the median age in the statins group was slightly higher than in the non-statins group (67.5 y vs. 61.7 y). In the statins group, 30 patients were treated with atorvastatin and 2 patients were treated with rosuvastatin. Compared with the non-statins group, the statins group had a significantly higher incidence rate of diabetes (31.0% vs. 59.4%, p = 0.014), while a significantly lower incidence rate of malignant tumors (31.0% vs. 9.4%, p = 0.025).
Table I
Clinical features of patients with SA bloodstream infection
Although the 30-day attributable mortality and 30-day all-cause mortality rate was higher in the non-statins group, no statistically significant difference was observed for the two groups (non-statins group 11.9%, statins group 6.3%, p = 0.410; non-statins group 14.3%, statins group 9.4%, p = 0.522).
Resistance of SA between the two groups
All the 74 SA strains were sensitive to vancomycin, linezolid and daptomycin, and the resistance rates of erythromycin and clindamycin were more than 35% in the two groups. There was no significant difference in two groups except for oxacillin and cefazolin. The incidence of MRSA in the non-statins group was significantly higher than in the statins group (non-statins group 38.1% vs. statins group 15.6%, p = 0.034) (Table II).
Table II
Antibiotic resistance of SA to antimicrobial agents, n (%)
Discussion
Our research indicated that the mortality in the statins group tended to be lower compared to the non-statins group, but no significant difference in the 30-day attributable mortality and 30-day all-cause mortality rate was noted. This research result is consistent with the studies by Yang and Fernandez [10, 11], however, it contradicts the previous reports for the advantages of statins in improving mortality by Liappis et al. and Masana et al. [8, 9]. The results of the study could be influenced by various confounding factors including an insufficient sample size, underlying disease status of the exposed population, age, and different types of statins. Therefore, further studies with a strong level of evidence are needed.
As for the antibiotic resistance test, the incidence of MRSA in the statins group was significantly lower than in the non-statins group. Except for erythromycin and clindamycin, the resistance rate of most drugs in the statins group was generally lower than in the non-statin group. It has been reported that statins could inhibit the oligomerization of penicillin binding protein 2a (PBP2a) by affecting the components of functional membrane microdomains (FMM) of bacteria in cell membranes [14]. FMM play an important role in membrane protein anchoring, polymer formation, signal transduction and other aspects, including its interaction with PBP2a, which is related to the resistance of MRSA to β-lactam antibiotics. Statins depolymerize and lose the drug-resistant protein PBP2a from the cell membrane, and restore the sensitivity of MRSA to β-lactam antibiotics [15].
In the concomitant disease results, the statins group had a higher incidence rate of diabetes disease compared to the non-statins group. Diabetes is often associated with dyslipidemia and dyslipidemia will increase the possibility of receiving statins, which is similar to previous studies [9]. Besides, the proportion of malignant tumor patients in the statins group was lower than in the non-statins group with a significant difference. Many studies have confirmed that statins can reduce the incidence rate of endometrial cancer, ovarian cancer, esophageal cancer, gastric cancer and colorectal cancer [16, 17]. In addition, statins can also reduce the mortality of patients with esophageal cancer, gastric cancer, colorectal cancer, prostate cancer and breast cancer [17, 18].
There are certain limitations in this study: firstly, our study was retrospective with a small sample size, and unknown variables may affect the results. For instance, the enrolled patients limited to a few diseases such as cardiovascular disease and chronic kidney disease with potential use of statins. This may result in the inability to assess the differences in overall mortality rates among patients with other underlying diseases or those without any underlying diseases. Secondly, due to the special nature of retrospective analysis, we did not intervene whether patients receive statins or not and which kind of statins to use, therefore the effect of empirical therapy on clinical outcomes was not completely controlled in this study. Furthermore, only patients with SA were included in this study, other types of bacteria related to bloodstream infection were not analyzed, which may lead to a greater bias in the outcome of death. Future investigations including randomized controlled trials and susceptibility test of MRSA to statins are needed to reevaluate the efficacy of statins in the treatment of SA bloodstream infections, mortality outcomes, and changes in MRSA sensitivity.
In conclusion, statins had no significant effect on the death outcome in patients with bloodstream infection of SA, however, the incidence of MRSA was lower in the statins group.