Back pain is a prevalent issue among athletes, particularly in sports that demand high levels of flexibility, strength, and precise body control [1]. Rhythmic gymnastics, characterized by complex movements, high flexibility demands, and extended training hours, places significant strain on the musculoskeletal system, especially the spine [2]. Athletes in this discipline often experience persistent low back pain, which can hinder performance, reduce training efficiency, and, if untreated, lead to long-term musculoskeletal disorders [2, 3]. Given the demanding nature of the sport, it is crucial to understand the underlying causes of back pain in rhythmic gymnasts and explore effective treatments to manage and prevent its recurrence [4]. The etiology of back pain in rhythmic gymnastics is multifactorial. Repetitive movements, such as hyperextension of the spine, twisting, and high-impact landings, combined with a lack of sufficient muscle strength and stability in the core and lower back, contribute to the development of pain [5]. Additionally, prolonged periods of training without adequate recovery, poor posture, and muscle imbalances can exacerbate the strain on the spine, leading to both acute and chronic pain [6].
Postural treatment has gained attention as an effective intervention to address and prevent back pain in athletes, including rhythmic gymnasts [2]. These treatments focus on correcting alignment, improving posture, and enhancing spinal mobility and flexibility [7]. Postural therapies, such as the Mézières method and Isostretching techniques, aim to restore optimal body alignment by addressing muscular imbalances and improving the function of the core and spinal muscles [8]. By focusing on the relationship between posture and pain, these treatments seek to not only alleviate existing pain but also prevent future injury by promoting balanced movement patterns and reducing strain on the spine [9]. The importance of postural treatment in this population cannot be overstated. Correcting postural abnormalities and strengthening the supporting muscles of the spine can significantly reduce the risk of developing low back pain [10].
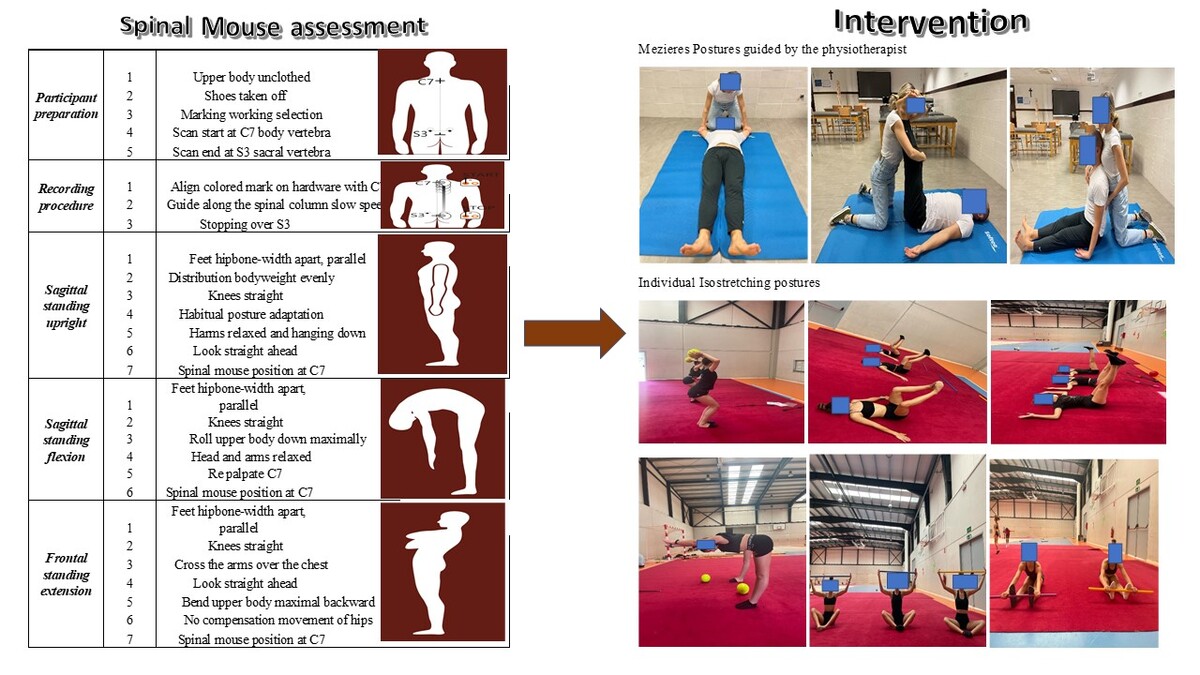
Therefore, the aim of this study is to evaluate the sagittal standing posture changes in rhythmic gymnasts with low back pain through the Spinal Mouse® digital instrument [11]. Specifically, the study aims to compare the impact of two different postural interventions – the Mézières method and Isostretching techniques – on improving spinal alignment, reducing pain intensity, and enhancing functional mobility in elite rhythmic gymnasts.
Methods
Design and sample
A randomized controlled trial was carried out to assess the effectiveness of two distinct postural treatments for elite rhythmic gymnasts experiencing low back pain, with a 12-week follow-up period and evaluations conducted at the start as well as at 2 and 4 weeks. A minimum of 20 elite gymnasts with low back pain were recruited for this trial. All participants were informed about the study and were free to withdraw at any time if they wished. Athletes provided written informed consent to ensure the protection of their rights. The intervention was conducted at the training camp. The trial was pre-registered on ClinicalTrials.gov under ID NCT05149703 and received ethics committee approval of the Catholic University of Murcia San Antonio UCAM with ID CE102105, in compliance with the latest revision of the Declaration of Helsinki. A statistician not involved in the study randomized the participants by generating a numbered list using a computer program, ensuring equal allocation frequency. The team trainer distributed the allocation sequence to all participants in sealed envelopes, which were opened immediately after completing the baseline assessments. To be eligible for this trial, participants had to be elite athletes diagnosed with persistent low back pain, aged 15 to 30 years, training at least 7 h, three times per week, with a pain intensity of 3 to 8 points on the Numeric Rating Scale (NRS), and be members of a national competitive rhythmic gymnastics team. Exclusion criteria included chronic diseases, acute musculoskeletal injuries, fractures, spondylolysis, and spondylolisthesis.
Assessments
Spinal curvatures, mobility, and functionality were measured using the Spinal Mouse® which offers a non-invasive, radiation-free, and highly adaptable method for assessing spinal posture and mobility in both static and dynamic conditions, making it an ideal tool for this population. Unlike static imaging, the Spinal Mouse® enables the evaluation of spinal curvatures during functional tasks, such as forward flexion or extension, which mimic the dynamic movements performed by gymnasts [12]. This capability is essential for identifying subtle, sport-specific patterns of spinal loading and dysfunction that may be missed in traditional assessments.
The Spinal Mouse® has demonstrated high reliability and validity in measuring spinal curvature, with studies indicating strong correlations with radiographic findings. It can assess spinal alignment in both standing and sitting positions, providing dynamic data during functional tasks such as forward flexion or extension, which are crucial for understanding the biomechanical behavior of the spine [12]. Additionally, its non-invasive nature and real-time data acquisition allow for an efficient and patient-friendly approach to posture evaluation without the limitations posed by traditional imaging modalities.
The Spinal Mouse® is manually guided along the spine to assess its curvatures and mobility. The specialized software displays the measurements on-screen in real time. The collected data is displayed on-screen, allowing for comparison with standard values and enabling an in-depth analysis that highlights areas of hypo- and hypermobility. In this trial, the Spinal Mouse® was used to measure the sagittal standing upright, sagittal standing flexion, and sagittal standing extension. Supplementary Material 1 provides a detailed, illustrated protocol for measuring the spinal vertebrae in sagittal standing postures.
Intervention
Two postural treatments were implemented in this trial, based on the group randomization. The experimental group received the Mézières treatment, while the active comparator group underwent six Isostretching postures, both guided by the same therapist with 10 years of experience in postural treatment. The basis for this comparison lies in their shared theoretical foundation in global postural reeducation and their emphasis on muscular elongation and postural correction [2, 13]. However, while both approaches aim to enhance flexibility, alignment, and neuromuscular control, they differ in their execution and biomechanical principles. Isostretching incorporates dynamic breathing patterns and integrates core activation throughout movement sequences, whereas the Mezieres method focuses on prolonged static postures to release compensatory tensions [14–17].
The Mézières treatment involves postural maintenance for approximately 30–60 min, while the Isostretching postures require a total of 90 s for active positioning. In this study, the most similar positions were selected for both treatments. The experimental group maintained the Mézières postures twice a week for 12 consecutive weeks, with each session lasting 30 min. No more than one posture was applied in a single session. In total, three postures were implemented. Specifically, the three postures implemented were: a) the gymnast in a supine position, b) the gymnast in a supine position with upper extremities abducted to 120°, and c) the gymnast in a sitting/supine position with hips flexed at 90°.
The active comparator group received six Isostretching postures, each individually maintained during 30-minute sessions twice a week, totaling 24 sessions over 12 weeks. It was not necessary to follow the same postural order, but it was essential to perform all the postures with a duration of 90 s each (30 s for 3 repetitions). If possible, the same posture could be held consecutively for 90 s, depending on the elite level of the athletes, their facility, and the elasticity of the gymnasts.
Mézières method and Isostretching are similar and different treatments at the same time. While Mezieres is an assisted active treatment, Isostretching is a fully active treatment. Specifically, in the Mézières method of the experimental group, the therapist taught and corrected the positioning and the patient accompanied the technique with deep breathing, isometric contraction, and proprioception. The same therapist guided the baseline and observed the Isostretching postures, in the comparator group, while the athletes tried to self-correct and autonomously followed the protocol of these positions with an adequate breathing and without the assistance or help of the therapist. Specifically, the guide was carried out as a group, so all gymnasts had the same information at the same time. Details and directions on how to proceed with each pose were given to each participant in the Isostretching group. The postural treatment illustration was outlined in Supplementary Material 2.
Statistical analysis
An a priori sample size calculation for each of the two groups was performed using G*Power 3.1.9.2 and the following parameters: ANOVA repeated measures within-between interaction as the statistical test, an effect size of 0.5 (medium), an α of 5%, and 75% power. It was estimated that 8 participants were required in each group. The baseline data analyses were performed using SPSS 25.0 for Windows (SPSS Inc, Chicago, IL). Mean and standard deviation were used to describe continuous and categorical variables, respectively. Data were assessed for normality and homogeneity of variance. Between group differences for baseline characteristics were explored using an independent sample Student’s t-test. The two-way ANOVA was performed with the GraphPad Prism program (version 8; GraphPad Software Inc). A correlation coefficient (ICC; two way random) and respective 95% confidence interval were used. Post hoc comparisons (Bonferroni) were performed when a significant main effect was found for time. A significant level was set at p < 0.05.
Results
A total of 17 elite gymnasts experiencing low back pain took part in the trial, with 8 athletes assigned to the Mézières group. The anthropometric data for both study groups are presented in Table I. No statistically significant differences were observed between the participants in terms of age, body mass index (BMI), or training hours per day and week (p > 0.05).
Table I
Anthropometric characteristics of elite athletes
Descriptive data
Table II presents the descriptive data for regional vertebral grades across the three postures, as assessed using the Spinal Mouse® instrument. No significant differences were found between the groups for the three analyzed postures, except for the L3-L4 and lower spine Th12 length, where a difference was observed with p < 0.05.
Table II
Sagittal standing postures representing regional vertebral characteristics
Sagittal standing upright posture
The analysis of the sagittal standing upright posture using two-way ANOVA revealed significant differences between groups, over time, and in combination (Figure 1 A). Significant group differences were observed across thoracic (Th3-Th4, Th6-Th7) and lumbar (L3-L4, L5-S1) regions, as well as in regional parameters like length and sacrum-hip vertebra (p < 0.05 in all variables). Longitudinal changes were most prominent at Th1-Th2 for the time-related changes analysis. Th7-Th8 vertebra, regional inclination, and regional thoracal spine fixed at Th12 showed significant differences between groups and over time with p < 0.05, suggesting dynamic variations in posture.
Sagittal standing flexion posture
Figure 1 B presents a detailed graphical analysis of the sagittal standing flexion posture where prominent differences were found in thoracic (Th7-Th8, Th12-L1) and lumbar regions (L1-L2, L2-L3), as well as in regional parameters like inclination and sacral-hip vertebra. As per time-related changes, longitudinal differences (p < 0.05) were noted at Th2-Th3 and Th5-Th6 vertebra.
Referring to the combined effects, Th8-Th9 [F (4, 60) = 3.619, p = 0.010] and Th9-Th10 [F (4, 60) = 2.537, p = 0.049], as well as regional length [F (4, 60) = 3.044, p = 0.023] and regional thoracal spine (fixed at Th12) [F (4, 60) = 6.900, p < 0.001] showed significant differences between groups and over time, indicating a dynamic postural adaptation.
Sagittal standing extension posture
Figure 1 C shows the sagittal standing extension posture. Most significant differences with p < 0.05 were seen in thoracic and lumbar levels, with particularly strong effects at Th12-L1 and regional parameters (inclination, lumbar spine, sacral-hip vertebra).
Referring to time-related changes, time effects were observed at Th6-Th7 [F (4, 60) = 2.572, p = 0.047]; Th7-Th8 [F (4, 60) = 3.323, p = 0.015]; Th10-Th11 [F (4, 60) = 3.432, p = 0.014] and L4-L5 [F (4, 60) = 2.964, p = 0.027] indicating longitudinal changes in posture.
Discussion
Referring to the sagittal upright posture, both Isostretching and the Mézières method demonstrated significant improvements in the participants’ ability to maintain proper alignment in that position. This result aligns with previous studies that emphasize the role of these methods in enhancing postural control through active elongation and muscle engagement [2, 7,8, 13, 14]. The Mézières method emphasizes restoring global muscle balance by addressing compensatory patterns that disrupt alignment [7, 8]. Similarly, Isostretching focuses on isometric contractions combined with controlled breathing to enhance proprioception and stability [13–17].
One possible explanation for their equivalence lies in the shared emphasis on elongation and controlled breathing. The Mézières method employs a holistic approach, aiming to reduce tension in overly contracted muscle chains, while Isostretching enhances awareness and control through targeted muscle activation [14, 15,17]. Both methods prioritize improving proprioceptive feedback mechanisms, which are crucial for maintaining static upright posture. These shared principles likely contribute to their comparable outcomes.
Isostretching is considered novel due to its unique integration of postural reeducation, controlled breathing, and core activation within a dynamic stretching framework. Unlike traditional flexibility training methods commonly used in gymnastics, which often emphasize passive or ballistic stretching [18], isostretching promotes active elongation of muscle chains while maintaining spinal alignment and neuromuscular engagement [19].
In sagittal stand upright flexion, both methods demonstrated significant improvements in participants’ ability to achieve controlled and pain-free forward bending. This is particularly noteworthy given the mechanical and neuromuscular challenges associated with flexion, such as lumbar strain and hamstring tightness.
The sagittal upright extension posture, characterized by backward bending, presents unique challenges due to the inherent stiffness or hypermobility of the thoracic and lumbar spine. Both interventions demonstrated equivalent efficacy in improving participants’ ability to achieve and sustain a controlled extension posture.
When comparing our findings to those of Grosdent et al., who investigated the effects of static postural training and proprioceptive exercises in gymnasts, both studies reported improved postural control. However, unlike the static approach used in their study, isostretching provided additional benefits in terms of dynamic stability, likely due to its integration of controlled breathing and core engagement during movement. This suggests that isostretching may be a more functional approach for athletes requiring both postural endurance and movement efficiency [20].
Lino et al. examined the effects of postural re-education through global postural stretching and reported decreased spinal misalignment and improved flexibility. While their findings are consistent with our results, our study extends this knowledge by demonstrating that isostretching, as a more dynamic form of global postural training, can further enhance core stability and movement efficiency – two critical factors for athletic performance [19].
Although this study provides robust evidence for the equivalence of Isostretching and the Mézières method, several limitations warrant consideration. The study’s sample size may limit the generalizability of the findings to broader populations as per elite athletes. Future studies with larger and more diverse cohorts are necessary to validate these results.
The study focused exclusively on sagittal plane postures. While these movements are crucial for functional alignment, future research should explore the impact of these interventions on other planes of movement, such as lateral flexion and rotation, to provide a more comprehensive understanding of their efficacy.
In conclusion, the present study highlights the comparable efficacy of Isostretching and the Mézières method in improving sagittal plane position, including upright standing, flexion, and extension. By emphasizing elongation, muscle chain balance, and mindful movement, both methods are equally effective and offer practical solutions for addressing postural dysfunctions. These findings underscore the importance of personalized, evidence-based approaches in musculoskeletal rehabilitation and posture correction, paving the way for further exploration of their applications in diverse populations and clinical settings.