Psoriasis and psoriatic arthritis (PsA) are chronic inflammatory immune-mediated entities that affect a substantial proportion of the Western population. In both entities, different comorbid conditions are reported, of which the most relevant and frequent are those of cardiovascular type [1, 2]. Cardiometabolic comorbidity (CC) is an important prognostic factor and is also associated with poorer responses and lower drug retention rates in psoriatic disease [1, 2]. However, the information we currently have about the relationship between CC and the negative impact of the disease on quality of life is scarce. Hence, our objective was to analyze the relationship between disease impact and CC in long-lasting PsA patients undergoing systemic treatment.
Post hoc analysis of the MAAPS (Minimal Activity in Psoriatic Arthritis) study (Spanish acronym for minimal activity in PsA) was performed. The main results, methodological details, and ethical considerations of the MAAPS study have been published elsewhere [3]. For the assessment of disease impact on patients’ lives, we used the 12-item Psoriatic Arthritis Impact of Disease (PsAID-12) questionnaire [4]. The PsAID-12 includes the following items: pain, fatigue, skin problems, work and leisure, disability for daily activity, the sensation of discomfort and irritation, sleep difficulties, disease coping, anxiety and uncertainty, embarrassment, social participation and depression. Each item has a particular weight, and the global score ranges from 0 (best status) to 10 (worst status). A PsAID score below 4 is established as a low disease impact (LDI) status [4]. According to goodness of fit tests, Student’s t-test, the Mann-Whitney U test, and the Kruskal-Wallis H-test were used to compare quantitative variables, and Pearson’s χ2 test or Fisher’s exact tests was used for qualitative variables. Data were analyzed using SPSS V19.0 statistical software.
A total of 227 patients were included but a complete data set was available for 223 patients. Among the latter, 122 (54.7%) were in LDI status. Mean time of disease evolution was not significantly different between LDI (9.6 ±7.9 years) and non-LDI patients (9.7 ±7.7 years). On the other hand, mean age was not different between the LDI (54.5 ±12.7 years) and non-LDI group (51.7 ±12.1 years). Table I shows the clinical characteristics of patients with a low and high disease impact.
Table I
Disease features between patients with low and high disease impact
[i] PsAID – psoriatic arthritis impact of disease, SD – standard deviation, BMI – body mass index, CRP – C-reactive protein, DIP – distal interphalangeal joint disease, PASI – psoriasis area and severity index, HAQ – Health Assessment Questionnaire, MDA – minimal disease activity. *p < 0.05, **p < 0.001.
At the study visit, 75.4% of LDI patients were receiving conventional disease-modifying antirheumatic drugs (DMARD) compared to 76.2% among non-LDI subjects, while 45.9% of LDI patients were on biologic drugs (mostly TNF-α inhibitors) compared to 52.5% of non-LDI.
There were more smokers (almost 25%) among non-LDI compared to LDI patients (13%), p = 0.083. The habitual consumption of alcohol was similar in both groups (LDI: 8% vs. non-LDI: 9%). There was a similar percentage of patients having sedentary lifestyle among those who reached and did not reach an LDI (30.3% vs. 28.7%). Among patients who reached an LDI, 42.6% (n = 52) did not present CC factors, 33 (27%) had one, 16 (13%) had two, 11 (9.0%) had three and the remaining 8.2% (n = 10) had four or more CC factors. The number of CC factors was not different between the two groups.
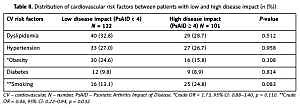
Arterial hypertension occurred in 27% of LDI compared to 26.7% of non-LDI patients. With respect to diabetes, almost 10% of patients in LDI status were diabetic compared to 9% of non-LDI. The distribution of dyslipidemia was similar in both groups (33% vs. 29%). There were more cases of hyperuricemia among LDI patients (15%) vs. non-LDI subjects (11%), p = NS. There was also a higher percentage of obese patients among those who reached the LDI status (24.6% vs. 15.8%), p = NS. Mean duration of the different cardiovascular comorbid factors was not statistically different between patients with and without LDI. There was a significantly higher frequency of coronary heart disease among LDI subjects (6.6% vs. 1%, p = 0.035; crude OR = 7.02, 95% CI: 0.86–57.1, p = 0.068). Table II shows the distribution of CC factors between patients with low and high disease impact. Table III displays similar information by age group.
Table II
Distribution of cardiovascular risk factors between patients with low and high disease impact (n (%))
| CV risk factors | Low disease impact (PsAID < 4) N = 122 | High disease impact (PsAID ≥ 4) N = 101 | P-value |
|---|---|---|---|
| Dyslipidemia | 40 (32.8) | 29 (28.7) | 0.512 |
| Hypertension | 33 (27.0) | 27 (26.7) | 0.958 |
| *Obesity | 30 (24.6) | 16 (15.8) | 0.108 |
| Diabetes | 12 (9.8) | 9 (8.9) | 0.814 |
| **Smoking | 16 (13.1) | 25 (24.8) | 0.083 |
Table III
Distribution of cardiometabolic risk factors and disease outcomes by age groups
| Variable | < 40 n = 31 | 40–49 n = 61 | 50–65 n = 60 | > 65 n = 75 | P-value |
|---|---|---|---|---|---|
| Disease duration, mean (SD) [years] | 6.2 (5.4) | 8 (5.8) | 8.4 (7.5) | 13.3 (8.9) | < 0.001 |
| Smokers (%) | 29 | 21.3 | 21.7 | 8 | 0.020 |
| Dyslipidemia (%) | 12.9 | 24.6 | 31.7 | 41.3 | 0.016 |
| Hypertension (%) | 0 | 9.8 | 26.7 | 53.3 | < 0.001 |
| Obesity (%) | 12.9 | 14.8 | 26.7 | 25.3 | NS |
| Diabetes (%) | 0 | 0 | 11.7 | 21.3 | < 0.001 |
| DAPSA rem. (%) | 25.9 | 33.3 | 20 | 29.3 | NS |
| PsAID < 4 (%) | 10.7 | 27 | 24.6 | 37.7 | < 0.05* |
With the exception of smoking, we found no clear association between disease impact and CC. The prevalence of coronary heart disease was even higher among patients who had reached an LDI situation. Among the CC factors evaluated, the only one that was more prevalent among patients who did not achieve the LDI status was smoking. Thus, PsA smokers had decreased odds of reaching a low-impact disease by 54% (crude OR = 0.46, 95% CI: 0.22–0.94, p = 0.032). Moreover, patients over 65 years of age had the lowest smoking rate (8%) but at the same time the highest frequency of an LDI state (37.7%). In contrast, patients younger than 40 years had the highest smoking rate (29%) but the lowest frequency of an LDI state (10.7%). All this is in keeping with the results of the Danish nationwide DANBIO registry in which PsA smokers had worse baseline patient-reported outcomes, shorter treatment adherence and poorer response to TNF-α blockers compared to non-smokers [5].
The concept of disease impact is multidimensional and may encompass various aspects that patients may relate or not to the effectiveness of treatments or the comorbidities linked to the disease [6]. This should lead us to a cautious interpretation of the results of our study, but also of those other studies that associate a benefit in the intervention on CC factors and PsA outcomes [7–10].
Our study has the limitations of a cross-sectional study, and perhaps it is not the most appropriate to test the association between CC and the impact of the disease measured by the PsAID. However, the information provided here has the strengths of a multicenter representative sample of patients treated under real-practice conditions.
With the exception of smoking, we found no clear association between CC and disease impact. All in all, patients with PsA should be encouraged and oriented to maintain healthy cardiovascular habits.