Introduction
Breast cancer is the most common malignant tumour with the highest incidence in women, and its incidence is gradually increasing [1]. Although the precise treatment of breast cancer is presently being pursued, precise treatment remains inseparable from accurate preoperative diagnosis. The breast biopsy methods in the 2018 National Comprehensive Cancer Network (NCCN) guidelines include fine-needle aspiration (FNA) biopsy, core needle biopsy, excisional biopsy, and vacuum-assistant biopsy [2].
Core needle biopsy is easy to operate and cheap. However, it can easily lead to acquiring inadequate samples and has a high pathological underestimation rate [3, 4]. Furthermore, repeated puncture leads to haematoma.
Vacuum-assisted Mammotome biopsy can obtain sufficient samples without repeated puncture. Hence, the diagnostic accuracy is high [5, 6]. However, it requires expensive special equipment (vacuum pumps, operating handles, etc.), and this technology also has a high incidence of haematoma [7].
In 2012, a wireless vacuum-assisted biopsy device was invented. Bagnera et al. [8] first confirmed the safety, convenience, and ease of operation of an elite biopsy device. Subsequently, Choi et al. [9] confirmed that the biopsy method has a high accuracy.
The elite biopsy system is a special vacuum-assisted, minimally invasive breast biopsy tool developed on the basis of a Mammotome minimally invasive rotary cutting system. This device is portable, does not need to be connected to a power supply, and is a special negative pressure device and special machine. The sampling can begin after self-examination on the basis of properly installing the biopsy needle and operating handle. Sufficient samples can be obtained with only one puncture. Furthermore, the accuracy of elite biopsy is high (95–97.6%) [10, 11]. The elite biopsy device has high accuracy and is convenient to operate. However, the clinical application of elite biopsy is rare. Hence, in order to further explore the elite biopsy method, the investigators designed the present test to compare the advantages and disadvantages of the three biopsy methods.
Material and methods
Age of subjects and experimental design
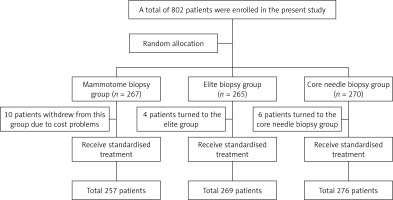
A total of 802 eligible patients, who were admitted to our department from January 2017 to January 2018, were enrolled in the present study. These lesions were measured by colour Doppler ultrasonography before the operation, regardless of the age and size of the masses. All patients were assessed by imaging. The diagnosis of BI-RADS by colour Doppler ultrasound or molybdenum target was grade 4 or higher. Patients with non-measurable lesions and patients with recurrence and metastasis detected by colour Doppler ultrasonography were excluded. All patients provided signed, informed consent for the biopsy. All biopsy procedures were performed by experienced clinicians. All patients were randomly divided into three groups: elite, Mammotome, and core needle biopsy groups. Among these patients, 267 were assigned to the Mammotome biopsy group (10 patients withdrew from this group due to cost problems, 6 patients transferred to the core needle biopsy group, and 4 patients transferred to the elite biopsy group). Furthermore, 265 patients were assigned in the elite biopsy group, while 270 patients were assigned to the core needle biopsy group. The age of patients in the study groups ranged from 20 to 85 years old, and the diameter of the lesion ranged from 0.68 to 6.0 cm under colour Doppler ultrasound. Standard treatment was performed after biopsy. The preoperative biopsy and postoperative pathology of each patient were compared, and the pathological underestimation rate and diagnostic coincidence rate of these three biopsy methods were calculated. The number of patients with haematoma after biopsy was counted, and the incidence of haematoma in these three groups was calculated. The cost was evaluated based on the standard of our hospital, and the costs of these three biopsy methods were roughly calculated (Figure 1, Table I).
Table I
The basic characteristics of the three groups
| Item | Mammotome biopsy group (n = 257) | Elite biopsy group (n = 269) | Core needle biopsy group (n = 276) |
|---|---|---|---|
| The size of tumour, n (%): | |||
| ≤ 2 cm | 129 (50.2) | 134 (49.8) | 139 (50.4) |
| 2 < D ≤ 5 cm | 118 (46.0) | 126 (46.8) | 128 (46.4) |
| > 5 cm | 10 (3.8) | 9 (3.4) | 9 (3.2) |
| Age [years], median | 53 ±9.1 | 54 ±9.5 | 54 ±9.3 |
| Puncture for the first time, n (%): | |||
| Yes# | 255 (99.2) | 267 (99.3) | 273 (98.9) |
| No | 2 (0.8) | 2 (0.7) | 3 (1.1) |
| Enlarged lymph nodes in the axilla, n (%): | |||
| Yes | 92 (35.8) | 96 (35.7) | 99 (35.9) |
| No | 165 (64.2) | 173 (64.3) | 177 (64.1) |
| Colour Doppler ultrasound BI-RADS grade, n (%): | |||
| Grade 3a | 16 (6.2) | 17 (6.3) | 17 (6.2) |
| Grade 4A | 35 (13.6) | 37 (13.8) | 38 (13.8) |
| Grade 4B | 40 (15.6) | 42 (15.6) | 43 (15.6) |
| Grade 4C | 87 (33.9) | 91 (33.8) | 94 (34.0) |
| Grade 5 | 79 (30.7) | 82 (30.5) | 84 (30.4) |
| Pathology results, n (%): | |||
| Invasive carcinoma | 193 (75.1) | 196 (72.9) | 183 (66.3) |
| DCIS | 15 (5.8) | 14 (5.2) | 8 (2.9) |
| Non-malignant diseases& | 48 (18.7) | 50 (18.6) | 48 (17.4) |
| Malignant tumor£ | 1 (0.4) | 3 (1.1) | 9 (3.3) |
| Undetermined* | 0 | 5 (1.8) | 27 (9.8) |
| Lymphoma | 0 | 1 (0.4) | 1 (0.3) |
Major instruments
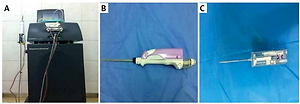
The ultrasound machine was a colour ultrasound diagnostic apparatus (LOGIQ BOOK XP, GE, USA), with a probe frequency of 11 MHz. The Mammotome biopsy system was purchased from Devicor Medical (USA), which included a vacuum suction pump, an operating handle, and a disposable 8 G biopsy rotary cutting (probe) needle head (the external diameter was 4.3 mm). The elite biopsy system was purchased from Devicor Medical (USA), which included an operating handle and a disposable 10 G biopsy rotary cutting (probe) needle head (the external diameter was 3.4 mm). The tissue biopsy needle was a disposable 14 G automatic biopsy needle (the external diameter was 2.1 mm) (CareFusion, USA) (Figure 2).
Operation methods
Mammotome biopsy
Patients were laid in the supine position, routine disinfection was performed, and surgical drapes were placed. The locations of the lesions were determined by ultrasound. The biopsy points were selected according to the requirements of the breast conserving surgery. It should be considered that the biopsy point and biopsy needle track should be removed as much as possible during the operation. Patients were treated with a mixture of 0.16% lidocaine and a small amount of epinephrine hydrochloride for local infiltration anaesthesia. Anaesthetics were injected into the posterior breast space and the surrounding area of the mass, in order to separate the pectoral muscles and reduce secondary damage. A Mammotome rotary cutting machine was checked and connected, and an incision of approximately 3-mm length was made at the appropriate position. The Mammotome rotary cutting knife head was inserted into the centre of the mass through the incision under the guidance of ultrasound, and the gland tissues were cut in a rotary way under ultrasound monitoring. An appropriate amount of tissue was obtained, and the rotary cutting step was ended. The biopsy tissue was fixed with 10% formalin for routine pathological examination. The surface of the wound was covered with sterile dressing and compressed for 15–30 min. Then, the compression bandage with elastic dressing was given for 48 h.
Core needle biopsy
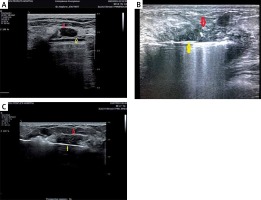
Routine disinfection was performed and surgical drapes were placed in the operation scope. The biopsy point was selected, and the infiltration anaesthesia of the skin and surrounding area of the mass was performed. Real-time monitoring was performed with a probe to optimise the location of the biopsy guide line and biopsy site. Then, the probe was fixed, and the biopsy needle was placed in the lesion position. Afterwards, the biopsy gun was initiated, and the biopsy needle was quickly pulled out after hearing the gunshot. The tissues in the needle groove were pushed out. This procedure was repeated to obtain the appropriate amount of tissues. Then, the specimens were fixed and patients were bandaged (Figure 3).
Evaluation criteria
Paraffin section pathological diagnosis was performed on both the biopsy and operation samples of the same patient. Haematoxylin and eosin (H&E) staining was performed. These paraffin sections were observed by two veteran physicians in the Department of Pathology, and their matching conclusion was regarded as the diagnosis. The diagnostic result of the surgical pathology was regarded as the gold standard. In the present study, the underestimation rate was defined as the percentage of the number of patients with benign or undetermined biopsy pathology but with malignant post-operative pathology (ductal carcinoma in situ (DCIS), invasive carcinoma, other malignant tumours), plus the number of patients with DCIS biopsy pathology but with invasive carcinoma post-operative pathology, which accounted for the total number of patients with non-invasive carcinoma or malignant tumour biopsy pathology. The diagnostic accordance rate was defined as the percentage of the number of patients with benign and malignant biopsy pathology, which was consistent with the post-operative pathology, and this accounted for the number of patients without undetermined biopsy pathology. The incidence of haematoma was defined as the percentage of the number of patients with haematomas, which accounted for the total number of patients in the present study.
Statistical analysis
Data were statistically analysed using SPSS 19.0 software. Count data were expressed in percentage (%) and compared using the χ2-test. If the theoretical frequency is between 1 and 5, the continuity correction result was used. If the theoretical frequency is less than 1, the Fisher exact probability test result was used. On the basis of the results of the χ2 test, the Bonferroni correction method was used to correct the results of multiple tests after the pairwise comparison. P < 0.05 was considered statistically significant.
Results
Pathological underestimation rate and diagnostic accordance rate
There were 257 patients in the Mammotome biopsy group. Among these patients, the biopsy diagnosis revealed that 193 patients had invasive carcinoma, 1 patient had a malignant tumour, 15 patients had DCIS, and 48 patients had non-malignant diseases (one of these patients was diagnosed with malignancy after the operation). The diagnostic accordance rate between the biopsy pathology and post-operative pathology was 99.6%, and the pathological underestimation rate was 1.6% (1/63).
There were 269 patients in the elite biopsy group. Among these patients, the biopsy diagnosis revealed that In total, 196 patients had invasive carcinoma, 3 patients had malignant tumours, 1 patient had lymphoma, 14 patients had DCIS (one of them was diagnosed with invasive carcinoma after the operation), 5 patients could not be diagnosed (two of them were diagnosed with malignancies after the operation), and 50 patients had non-malignant diseases (two of them were diagnosed with malignancies after the operation). The diagnostic accordance rate between biopsy pathology and post-operative pathology was 98.9% (261/264), and the pathological underestimation rate was 7.2% (5/69).
There were 276 patients in the core needle biopsy group. Among these patients, the biopsy diagnosis revealed that 183 patients had invasive carcinomas, 8 patients had DCIS (all of them were diagnosed with invasive carcinoma after the operation), 27 patients could not be diagnosed (18 of them were diagnosed with breast cancer after the operation), 48 patients had non-malignant diseases (5 of them were diagnosed with breast cancer after the operation), 9 patients had malignant tumours, and 1 patient had lymphoma. The diagnostic accordance rate between the biopsy pathology and post-operative pathology was 94.7% (236/249), and the pathological underestimation rate was 37.3% (31/83).
There were differences in overall comparison in terms of diagnostic accordance rates and pathological underestimation rates among the three groups (p < 0.001). The diagnostic accordance rates of the elite biopsy group (98.9%) were significantly higher than those of the core needle biopsy group (94.7%), and the difference was statistically significant (p = 0.003). The diagnostic accordance rates of the Mammotome biopsy group (99.6%) was significantly higher than that of the core needle biopsy group (94.7%), and the difference was statistically significant (p < 0.001). The difference in diagnostic accordance rates between the Mammotome biopsy group and elite biopsy group was not statistically significant (p = 1.905). The pathological underestimation rates of the elite biopsy group (7.2%) was significantly lower than that of the core needle biopsy group (37.3%), and the difference was statistically significant (p < 0.001). The pathological underestimation rates of the Mammotome biopsy group (1.6%) was significantly lower than that of the core needle biopsy group (37.3%), and the difference was statistically significant (p < 0.0001). The difference in pathological underestimation rates between the Mammotome biopsy group and the elite biopsy group was not statistically significant (p = 0.762, Table II).
Table II
Comparison of biopsy and postoperative pathology
In subgroups, different colour Doppler ultrasound BI-RADS grade had different results. In respect of diagnostic accordance rates, only grade 4B was statistically significant as a whole (p = 0.002). In the subsequent pairwise comparison, the diagnostic accordance rate of the elite biopsy group was significantly higher than that of the core needle biopsy group, and the difference was statistically significant (p = 0.006). The diagnostic accordance rate of the Mammotome biopsy group was significantly higher than that of the core needle biopsy group, and the difference was statistically significant (p = 0.048). The difference in diagnostic accordance rates between the Mammotome biopsy group and the elite biopsy group was not statistically significant. In respect of pathological underestimation rates, grades 4B, 4C, and 5 were statistically significant as a whole (p < 0.001). In subsequent pairwise comparison of grade 4B, the rate of the elite biopsy group was significantly lower than that of the core needle biopsy group, and the difference was statistically significant (p = 0.024). The rate of the Mammotome biopsy group was significantly lower than that of the core needle biopsy group, and the difference was statistically significant (p < 0.001). In following pairwise comparison of grade 4C, the rate of the elite biopsy group was significantly lower than that of the core needle biopsy group, and the difference was statistically significant (p = 0.006). The rate of the Mammotome biopsy group was significantly lower than that of the core needle biopsy group, and the difference was statistically significant (p < 0.001). In following pairwise comparison of grade 5, the rate of the elite biopsy group was significantly lower than that of the core needle biopsy group, and the difference was statistically significant (p < 0.001). The rate of the Mammotome biopsy group was significantly lower than that of the core needle biopsy group, and the difference was statistically significant (p < 0.001). The rates between the Mammotome biopsy group and elite biopsy group were not statistically significant in these three subgroups (Table III).
Table III
The colour Doppler ultrasound BI-RADS grade of three groups
In the subgroup of the size of the mass it was significant only in 2 < D ≤ 5 cm about diagnostic accordance rate (Mammotome: 99.2%, elite: 99.2%, core needle: 93.0%, p = 0.004). However, there was no statistical difference between any two groups. There was significance in ≤ 2 cm (p = 0.002) and 2 < D ≤ 5 cm (p < 0.001) in terms of pathological underestimation rates. In subsequent pairwise comparison, the rate of the Mammotome biopsy group was lower than that of the core needle biopsy group in ≤ 2 cm (0.0 vs. 23.5), and the difference was statistically significant (p = 0.003). In 2 < D ≤ 5 cm, the differences of Mammotome vs. core needle (4.3 vs. 6.3) and elite vs. core needle (8.3 vs. 6.3) were significant (p < 0.001).
The incidence of haematoma
The case data were reviewed. There were 257 patients in the Mammotome biopsy group. Among these patients, haematoma occurred in 41 patients after the operation, and the incidence of haematoma was 15.9%. Furthermore, there were 269 patients in the elite biopsy group. Among these patients, haematoma occurred in 35 patients after the operation, and the incidence of haematoma was 13.0%. There were 276 patients in the core needle biopsy group. Among these patients, haematoma occurred in 60 patients after the operation, and the incidence of haematoma was 21.7%. There were differences in overall comparison among the three groups (p < 0.001). The incidence of haematoma in the elite biopsy group was lower than that in the core needle biopsy group, and the difference was statistically significant (p = 0.021). Nonetheless, the difference between the Mammotome biopsy group and core needle biopsy group was not statistically significant (p = 0.267), as was the case between the Mammotome biopsy group and elite biopsy group (p = 1.000, Table IV).
Table IV
The comparison of three groups after puncture
| Treatment | Mammotome biopsy group, n (%) | Elite biopsy group, n (%) | Core needle biopsy group, n (%) | P-value |
|---|---|---|---|---|
| Neoadjuvant therapy | 45 (17.5) | 47 (17.5) | 49 (17.7) | 0.9956 |
| Breast-conserving operation§ | 38 (17.9) | 47 (21.2) | 35 (15.4) | 0.285 |
| Mastectomy | 177 (64.6) | 175 (61.3) | 192 (66.9) | |
| Haematoma | 41 (15.9) | 35 (13.0) | 60 (21.7) | 0.0219 |
In the experiment, a small number of people gave up breast-conserving surgery because of the haematoma. A total of 16 patients gave up breast-conserving due to severe haematoma. The statistical results revealed that in the core needle biopsy group 10 patients gave up breast conserving, and the breast conserving rate was reduced by 4.4%. In the Mammotome biopsy group, 6 patients gave up breast-conserving due to hematoma, and the breast conserving rate was reduced by 2.8%. In the elite biopsy group, none of the patients gave up breast-conserving due to haematoma. Concerning patients resigned from BCT due to an extensive haematoma, there were differences in overall comparison among the three groups (p = 0.007). However, in pairings, only the difference between the elite biopsy group and core needle biopsy group was statistically significant (p = 0.012). The p-value between the Mammotome biopsy group and core needle biopsy group was 1.000. The p-value between the Mammotome biopsy group and elite needle biopsy group was 0.105.
Cost
With our hospital’s fee standard as a reference, the cost of a Mammotome biopsy is approximately 7500 yuan, the cost of an elite biopsy is approximately 2800 yuan, and the cost of a core needle biopsy is approximately 1600 yuan. The cost of Mammotome biopsy was much higher than that of elite biopsy and core needle biopsy.
Discussion
Ultrasound-guided core needle biopsy is an accurate method for evaluating breast masses [12], which has been widely used in clinics. However, due to its spring drive, its controllability in exciting moments remains poor. To master the technique, a biopsy operator needs to undergo a certain learning curve [13]. Therefore, the requirement of operation level of biopsy operators is high, the operator’s experience is closely associated to the reliability of the diagnostic results [14], and improper operation can easily cause secondary damages, such as pneumothorax [15]. The operation stability of vacuum-assisted biopsy is significantly higher than that of core needle biopsy, the secondary damage is less, and the amount of acquired tissue is large. Although there is a learning curve in the operation of vacuum-assisted biopsy, it is safe even in the early stages of the operation [16]. According to the length and weight of the biopsy specimen, the amount of tissue of the 14 G biopsy needle is approximately 12–17 mg, the amount of acquired tissue of the 11 G biopsy needle is approximately 83–116 mg, and the amount of acquired tissue of the 8 G biopsy needle is approximately 246–310 mg. It has been mentioned in the article that the amount of acquired tissue of the 11 G Mammotome probe is approximately six times that of the 14 G core needle [17]. Through our calculations, the amount of acquired tissue of the 10 G elite biopsy is 5–7 times that of the 14 G core needle, and the amount of acquired tissue of the 8 G elite biopsy is 14–25 times that of the 14 G core needle. An adequate amount tissue significantly affects the diagnostic accordance rate [6, 18]. Therefore, vacuum-assisted biopsy has a higher diagnostic accuracy rate and better safety, when compared to core needle biopsy [5]. Accurate preoperative diagnosis is essential for treatment decision-making. For patients with masses > 5 cm (T3), when the biopsy pathological diagnosis is invasive carcinoma, neoadjuvant therapy is the first choice for treatment. If the biopsy diagnosis is DCIS or DCIS with a small amount of invasive carcinoma, perhaps surgical therapy is the first choice. Therefore, high diagnostic accordance rate and low pathological underestimation rate are closely correlated with the formulation of the treatment plan and prognosis of patients. Our experimental results show that elite biopsy has a higher pathological accuracy rate and lower underestimation rate than core needle biopsy. There is no significant difference in pathological accuracy rate and underestimation rate between the Mammotome and elite biopsy group, as other experimental studies have revealed [11, 19]. It is safe to operate without special equipment, it is easy and simple to operate, and is not limited by the environment. The Mammotome’s line-piping system limits the needle insertion direction, needle insertion depth, and rotation direction to a certain extent, and has certain requirements for the operation site. Hence, elite biopsy has obvious advantages over Mammotome biopsy.
The biopsy results of different BI-RADS grades revealed that the difference in the diagnostic accordance rate of BI-RADS grade was statistically significant only in grade 4B among the three groups. In subsequent pairwise comparison, the difference between Mammotome biopsy and core needle biopsy, elite and core needle biopsy were significant. But, the differences in the pathological underestimation rates of BI-RADS grades 4B, 4C, and 5 among the three groups were statistically significant. Regardless of BI-RADS result, the rate of the elite biopsy group was significantly lower than that of the core needle biopsy group. The longitudinal comparison revealed that in our experiments there was no significant correlation between the BI-RADS grade and the accuracy of diagnosis and the rate of pathological underestimation. The study revealed that the accuracy of core needle biopsy increased with the increase in BI-RADS grade, but the difference was not statistically significant [20]. Maybe there is such a correlation; however, there are few experiments to confirm their correlation directly. BI-RADS is an index to assess the risk of breast cancer. Its height only represents the probability of breast cancer. Whether the accuracy of diagnosis and the rate of pathological underestimation are correlated to BI-RADS grade or not is worthy of further exploration. Hence, no matter the rating, we can choose the elite biopsy first. In view of the fact of the high diagnostic accordance rate of the three biopsy methods, and taking into account the cost, core needle biopsy can be considered for grade 4C and 5 masses.
Determining from the results of our experiments, the accuracy of the biopsy is not correlated to the size of the mass. Although some of the positive results were obtained in our experiment, there was no corresponding clinical significance. According to the ease of operation, a large mass is easier to operate than a small one. This difference is more pronounced in the core needle biopsy. For the incidence of haematoma, vacuum-assisted biopsy does not require repeated needle insertion, which reduces tissue secondary damage, and the incidence of haematoma is lower than that of core needle biopsy. The external diameter of the Mammotome biopsy needle is 4.3 mm, while the external diameter of the elite biopsy needle is 3.4 mm. The external diameter of the Mammotome biopsy needle is larger than that of the elite biopsy needle, which leads to more gland destruction during biopsy to the glands. In fact, the incidence of haematoma was statistically significant in only the elite group compared with core needle biopsy. The incidence of haematoma of the elite biopsy group was lower than that of the core needle biopsy group. In deciding the surgical method before the operation, there is a need to comprehensively evaluate the size of the mass, the size of the breast, and the ratio of the mass to the breast, and there is also a need to evaluate the operability of the breast-conserving surgery and the accuracy of the surgical margin selection. Severe haematoma can lead to unclear margins of the mass, which affects the judgment of the surgical margin. For patients with severe haematoma after biopsy, the incidence of false negativity is increased in breast-conserving surgical margins. Therefore, taking into account operation safety, in the preoperative formulation of surgical strategies, some of the patients gave up breast conserving because of the haematoma. The decreased rate of breast conserving in the elite group was significantly lower than that in the core needle biopsy group. This approach can improve the breast conserving rate. Related experimental studies have revealed that breast-conserving patients have better functional status and fewer symptoms than those with mastectomy [21]. The loss of breast has a major effect on patient’s identity and mental health. Patients who underwent breast-conserving therapy (BCT) reported better body shape. The results of the experiment showed that the approach of operation had little effect on the quality of life. After all, there are too many factors related to quality of life [22]. But the investigator wonders whether breast-preservation has a certain effect on marriage.
In conclusion, as a new method of breast biopsy, elite biopsy has a high diagnostic accuracy rate and a low pathological underestimate rate, and the incidence of haematoma after biopsy is low. Furthermore, this approach can improve the breast conserving rate, and has an affordable price. As an economical biopsy method with high accuracy and safety, elite biopsy can be widely used in clinics.